Common vaginal infections
- Dr Samantha Wild, Clinical Lead for Women's Health and Bupa GP
Vaginal infections are very common. They can cause symptoms, such as soreness, itching and changes in vaginal discharge. Getting medical advice as soon as you notice a problem can help to get rid of your infection quickly and prevent complications.
About common vaginal infections
Vaginal infections can be caused by bacteria, fungi, parasites or viruses. Some of these things normally live in your vagina without causing any problems. But sometimes they can grow out of control, causing an infection in your vagina and vulva (the area surrounding your vagina). Things that can trigger this or increase your risk include:
- being sexually active, especially if you’ve had a recent change in partner
- using vaginal hygiene products like douches, soaps, bubble baths, deodorants, vaginal washes and wipes
- taking antibiotics
- some types of contraception, including the copper intrauterine device (IUD)
- having a health condition that affects your immune system, like diabetes or HIV
- taking long-term steroid medicines
Some common vaginal infections are sexually transmitted infections (STIs). This means you can get them if you have unprotected sex with an infected person.
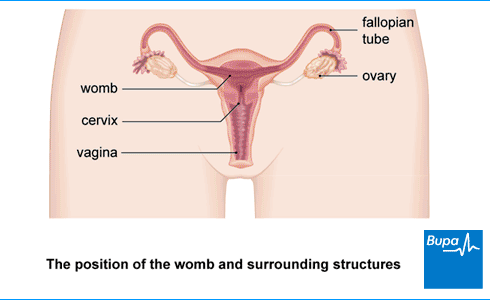
A vaginal infection isn’t the same as a urinary tract infection (UTI) or cystitis. A UTI affects your bladder, or the tubes that carry urine out of your body. Your vagina is part of your reproductive system. This is separate from your bladder and urinary tract.
Types of vaginal infection
Common vaginal infections include the following.
- Bacterial vaginosis. This is the most common vaginal infection. It happens when bacteria that normally live in your vagina grow out of control. It’s not sexually transmitted, but is linked to being sexually active. Bacterial vaginosis symptoms include a thin grey or white, fishy-smelling vaginal discharge.
- Chlamydia. This is the most common STI in the UK. It’s caused by a type of bacterium. Common symptoms include increased discharge, bleeding between periods or after sex, and pain when you pee or during sex.
- Genital herpes. These are caused by the human papilloma virus (HPV) and spread through sexual contact. The warts appear around your vulva, cervix, vagina or anus.
- Genital warts. These are caused by the human papilloma virus (HPV) and spread through sexual contact. The warts appear around your vulva, cervix, vagina or anus.
- Gonorrhoea. An STI caused by bacteria, gonorrhoea can cause an increase in discharge and pain around your lower abdomen. It might hurt when you pee, and you may get bleeding between your periods.
- Thrush. This is a common fungal infection. Common thrush symptoms include itching or soreness around your vulva and sometimes a thick, white vaginal discharge (a bit like cottage cheese).
- Trichomoniasis. This is an STI caused by a parasite (a tiny organism that lives on your body). If you have trichomoniasis, you may have a yellow-green, foul-smelling and possibly frothy vaginal discharge.
It’s possible to have more than one infection at a time. For example, if you have bacterial vaginosis, you’re at greater risk of getting chlamydia, gonorrhoea, genital herpes and trichomoniasis.
You can have vaginal symptoms, such as itching, without having an infection. It's also normal and healthy to have some discharge from your vagina. The amount and consistency of this discharge can change at different times. These include during your menstrual cycle, as you get older, if you take the contraceptive pill or if you get pregnant. But an abnormal change in your vaginal discharge, especially if you also have other symptoms, can be a sign of an infection.
See your GP if you think you may have a vaginal infection. You can also book an appointment directly with a genitourinary medicine (GUM) or sexual health clinic if you think you could have an STI. Your GP may also refer you here if they suspect you have an STI.
What should I do if I'm embarrassed to talk to my doctor?
Seeing a doctor when you're embarrassed | Watch in 2:08 minutes
Dr Naveen Puri talks about how to make it easier to see a doctor about a health issue when you are feeling embarrassed.
Hello, I am Dr Naveen Puri, I am one of the GPs within Bupa Health Clinics.
Today I want to speak to you about embarrassing problems you might have and what we can do if you attend one of our clinics.
I want you to know that many people feel embarrassed or concerned about speaking about certain things with their doctors, but I'm here to reassure you these are the kinds of things we deal with every day.
For me, looking at someone's bottom or their breasts or their genitalia is no different to looking at their nose or elbow.
And that's true for all doctors as we train for many years in these parts of the body and are very used to having these conversations with people just like you.
So what I would encourage you to do if you have any concerns from your perspective, be it a change in your bowel habit, be it a lump, a rash, a swelling. Something on your genitalia or a part of your body you're not particularly familiar with or feel uncomfortable discussing.
Please be assured your doctor has done it all before.
Some of the ways we find patients find it easier to speak to a doctor is to either tell the doctor you feel embarrassed up front. That way a doctor can make extra effort to make sure you feel comfortable.
Or some patients come to us with pieces of paper and will write the problem down and hand it to us. That way we can help with whatever is going on for you as well.
You may also find it helpful to ask for a specific doctor, someone you're familiar with in your practice. Or you might want to ask for a doctor of a specific gender, or background to your liking as well.
I'd also say, doctors do this every day so don't be alarmed if we ask you certain questions around your symptoms. It is purely so we can help you get the best outcome for your enquiry.
And then finally, feel free to use language that suits you as well. We don't expect you to know the medical words for things, or a name for your diagnosis. That's our job to find out for you.
So, take your time, see a doctor, and hopefully we can help put your mind at ease.
Diagnosis of common vaginal infections
Your doctor or nurse will ask you about your symptoms and medical history. Sometimes this is enough to understand what the problem is. They may also ask to examine your genital area. You’ll need to give your consent before a doctor or nurse can examine you. They will also offer you a chaperone (someone else who will stay in the room at the same time).
In an examination, the doctor or nurse will first look at your vulva (the area surrounding your vagina). They’ll then use an instrument called a speculum to gently open your vagina. This allows them to look and examine inside. They may take a sample of discharge or cells from your vagina using a small, round cotton bud called a swab. These samples are sent to a laboratory for testing.
Your nurse or doctor may also ask to take a urine sample. This is used to check whether you’re pregnant, or to rule out a urinary tract infection.
Treatment of common vaginal infections
Some vaginal infections, like genital warts, may eventually go by itself without treatment. But others, like chlamydia, gonorrhoea and trichomoniasis, can go on to cause serious complications if you don’t get them treated. These can include fertility problems, chronic pelvic pain from pelvic inflammatory disease and problems during pregnancy.
What treatment your doctor may recommend will depend on exactly what infection you have. That’s why it’s important to see your doctor or go to a sexual health clinic for a proper diagnosis.
Treatments may include the following.
- Antibiotics for bacterial vaginosis, chlamydia, gonorrhoea and trichomoniasis. These can quickly get rid of the infection. Usually, you’ll be prescribed antibiotics that you take by mouth for up to a week. But for bacterial vaginosis, you may have an antibiotic gel or cream that you apply to your vagina instead.
- Antiviral medicines for genital herpes. These may help to clear your blisters. You can’t get rid of the virus itself though – once you’re infected, it remains in your body. Your symptoms may flare up again if the virus is reactivated.
- Creams, ointments and solutions for genital warts. You may be able to apply these at home to help get rid of your warts. Sometimes you may need specialist treatment from your doctor to remove them.
- Antifungal tablets for thrush. You’ll usually only need to take a single tablet, although it can take a week or two for symptoms to go. You can also get creams or pessaries (which you put in your vagina), which you apply for two to three days. You can get these from a pharmacist without a prescription. But if you’re pregnant, see your GP.
Some people try using home remedies, such as live, natural probiotic yoghurt and tea tree oil to ease symptoms of thrush. But there’s no evidence to say whether these things can help.
Tea tree oil and other essential oils may irritate your skin and actually make your symptoms worse. It’s best to avoid using these.
Prevention of common vaginal infections
Many common vaginal infections are passed on through sexual contact with an infected partner. These include chlamydia, gonorrhoea, trichomoniasis, genital warts and herpes. Using a condom can provide good protection against many STIs. You should also have a test for STIs before having sex with someone new, and suggest they do too.
You can reduce your risk of some vaginal infections, like thrush and bacterial vaginosis, by avoiding using hygiene products in the area around your vagina. These include soaps, shower gels, bath additives, douches and vaginal washes. This is because these products can irritate your vagina and lead to infection.
Worried about your Period health?
A personalised care plan for heavy, painful or irregular periods for those 18 and over. Now available.
This will depend on the type of vaginal infection you have and how quickly you get treatment. For infections that are treated with antibiotics (such as bacterial vaginosis, trichomoniasis and chlamydia), you’ll usually need treatment for around seven days. For thrush, it may take up to a week or two after treatment for the symptoms to go.
Read more in our section on treatment of common vaginal infections.
If you have bacterial vaginosis, you may notice your vaginal discharge is thinner than normal and a grey or white colour. It may also smell ‘off’ or fishy. Bacterial vaginal infections also include sexually transmitted infections like chlamydia and gonorrhoea. These can cause other symptoms like pain when you pee or bleeding between periods or after sex.
See our types section for more details.
Trichomoniasis can cause a vaginal discharge that’s yellow-green, smells odd and can sometimes be frothy too. It’s a sexually transmitted infection caused by a parasite. You’ll need to get checked out by a doctor or nurse to be sure if trichomoniasis is causing your symptoms.
See the types section for more details.
Bacterial vaginosis tends to cause a thin, grey/white, fishy-smelling vaginal discharge. With vaginal thrush, the discharge is more likely to be thick and white. It can make you itch and feel sore too. If you haven’t had these symptoms before, it’s always best to get checked out by a GP or sexual health clinic. They can make sure you get a correct diagnosis.
See our diagnosis section for more on getting diagnosed.
Vaginal thrush
Sexually transmitted infections (STIs)
What is chlamydia?
Chlamydia is one of the most common sexually transmitted infections (STIs) in the UK. Dr Naveen Puri answers some very common questions about chlamydia.
What are genital warts?
Genital warts are a very common sexually transmitted infection. They’re caused by infection with the human papilloma virus (HPV). But are HPV and genital warts the same thing? And what do genital warts look like?
What is gonorrhoea?
Gonorrhoea is a type of sexually transmitted infection (STI). Alongside chlamydia, it is one of the most common STIs in the UK. Dr Naveen Puri explains more about this common STI.
What is HIV?
Human immunodeficiency virus (HIV) is a virus which affects your immune system. This is because it lowers the number of some types of cells in your body that fight disease.
Did our Common vaginal infections information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Vaginitis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 February 2023
- Candida – female genital. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2022
- Assessment of vaginal discharge. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 February 2023
- Vaginal discharge. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised January 2019
- Bacterial vaginosis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2018
- Urinary tract infection (lower) – women. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2023
- Chlamydia – uncomplicated genital. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2022
- Herpes simplex – genital. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised January 2023
- Warts – anogenital. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised November 2022
- Gonorrhoea. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2022
- Trichomoniasis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised May 2020
- Pruritus vulvae. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2022
- Guide to sexual health services. NHS. www.nhs.uk, last reviewed 14 September 2022
- Warts – anogenital. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised November 2022
- British Association for Sexual Health and HIV national guideline for the management of vulvovaginal candidiasis. British Association for Sexual Health and HIV. www.bashhguidelines.org, published 2019
- Sexual health and contraception. Sexually transmitted infection. Oxford handbook of general practice. Oxford Medicine Online. oxfordmedicine.com, published online June 2020
- Pippa Coulter, Freelance Health Editor



