Pelvic inflammatory disease
- Mr Yemi Kuponiyi, Consultant Obstetrician and Gynaecologist
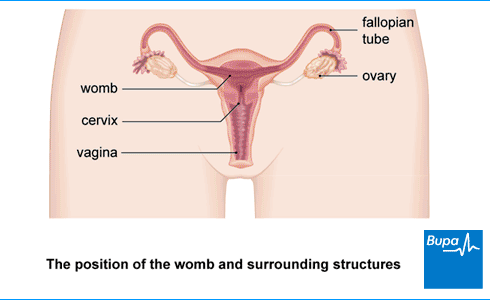
Pelvic inflammatory disease (PID) is an infection of your upper reproductive organs. These include your womb (uterus), ovaries and fallopian tubes. PID symptoms include:
- pain in your lower tummy
- an unusual vaginal discharge
- bleeding between your periods
- bleeding after you have sex.
About pelvic inflammatory disease
Pelvic inflammatory disease is most common in people with female reproductive organs aged between 20 and 24. It doesn’t always cause symptoms, so some people don’t realise they have it.
Pelvic inflammatory disease is usually treated with antibiotics but sometimes you may need treatment in hospital. If the pelvic infection is serious or you don’t get treatment, you could get long-term pain in your pelvis or fertility problems.
Causes of PID
Pelvic inflammatory disease (PID) is almost always caused by a sexually transmitted infection (STI). The most common infections that cause it are chlamydia and gonorrhoea. When you have this type of infection, bacteria in your vagina or cervix can move up to your womb, fallopian tubes and ovaries. This can cause pelvic inflammatory disease.
You may be more likely to get pelvic inflammatory disease if you have:
- had a STI or pelvic inflammatory disease before
- had unprotected sex with several partners
- had a new sexual partner (in the last three months)
- an intrauterine device (IUD, coil) particularly if you had it fitted within the last 4–6 weeks
- recently terminated a pregnancy (had an abortion)
Symptoms of PID
Pelvic inflammatory disease (PID) symptoms can be very mild or you may not have any symptoms at all.
If you do get PID symptoms, they may include:
- a dull, cramping or aching pain in your lower tummy – this might be on one or both sides or just on the upper right side
- an unusual vaginal discharge – it may be smelly
- bleeding between your periods or after you have sex
- uncomfortable or painful sex
- painful periods
- heavy periods
- a high temperature (over 38°C) (although your temperature may be normal)
- feeling or being sick
These symptoms can be caused by other health conditions, such as endometriosis or cystitis. But if you have them, it’s a good idea to get them checked by your GP or your local sexual health clinic. If you have pelvic inflammatory disease, it’s important to start treatment as soon as possible because treatment will reduce your chance of complications.
Diagnosis of PID
To diagnose pelvic inflammatory disease (PID), your GP will ask about your symptoms and your medical and sexual history. They’ll examine your vagina to check for signs of a pelvic infection.
Your GP may take some samples (swabs) from inside your vagina and cervix to test for bacteria and sexually transmitted infections. This is like having a cervical smear test and it may feel uncomfortable. But it’s important to get tested so you can get the treatment you may need.
You may have some other tests including a:
- blood test to check for infection
- urine test for chlamydia (using a sample of pee)
- urine test to rule out a urine infection
- pregnancy test – the symptoms of PID are similar to those of an ectopic pregnancy
If your symptoms are very bad, your GP may advise you to go to hospital for more urgent treatment.
If your GP isn’t sure if you have PID, they may refer you to a specialist for more tests. These tests may include:
- a transvaginal ultrasound scan, which creates a picture of the inside of your pelvis
- a laparoscopy, which is a keyhole procedure to look at your fallopian tubes, ovaries and womb
- more blood tests
- an MRI or CT scan
Treatment of PID
Self-help
If you have pelvic inflammatory disease (PID), you’ll need to see a GP for treatment.
If your symptoms are bad, get plenty of rest until you feel better. If you’re in pain, you can take over-the-counter painkillers, such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine. If you have any questions, ask a pharmacist for advice.
Antibiotics
Pelvic inflammatory disease (PID) treatment is with antibiotics, usually two or more different types. Your doctor will probably advise you to start taking antibiotics straightaway, rather than wait for test results. This is because the long-term effects of pelvic inflammatory disease can be serious, so it's best to start PID treatment as soon as possible.
Your GP might prescribe antibiotic tablets, which you’ll usually need to take for 14 days. It’s important to finish the whole course of antibiotics, even if you feel better, to make sure the infection clears up. Sometimes, your GP might also give you an antibiotic injection.
Make sure you (and your partner if you have one) finish the antibiotics before you have sex again (including oral sex). Or use a barrier method of protection, such as a condom.
If you don’t get better or your symptoms get worse after you’ve been taking antibiotics for two to three days, speak to your GP. You may need to go to hospital to have antibiotics through a drip.
If you have an intrauterine device (IUD) and antibiotics haven’t started to help after three days, your GP may suggest you have the IUD taken out.
If you’re pregnant, you’ll need to go to the hospital for antibiotics through a drip.
Surgery
If you have a severe infection or antibiotics through a drip don’t work, you may need to have a keyhole surgery procedure. This is to drain fluid from inside your fallopian tubes and wash out any infected fluid within your pelvis. A surgeon will use a needle to drain infected fluid – they’ll use an ultrasound scan to guide them to the right spot.
You may also need to have a procedure to remove some damaged tissue from inside your uterus. Your surgeon may do this in a laparoscopy.
Treating sexual partners
If you have pelvic inflammatory disease, your GP will test you for sexually transmitted infections (STIs), such as chlamydia and gonorrhoea. They’ll also ask you to tell any sexual partner (any you’ve had in the last six months) that you have pelvic inflammatory disease. Your past and present partners need to get tested and treated for these infections too. Staff at a sexual health clinic can contact your past partners for you.
Complications of PID
If pelvic inflammatory disease (PID) isn’t treated or isn’t treated quickly, it can cause complications. These include the following.
- An abscess (a collection of pus) can form on your ovary or fallopian tube.
- Ectopic pregnancy. A fertilised egg can implant outside your womb, usually in one of your fallopian tubes. To find out more, see our FAQ: Why is an ectopic pregnancy more likely if I have PID?
- Infertility. If PID damages your fallopian tubes, you may find it harder to get pregnant. PID is more likely to affect your fertility if it’s very bad or you’ve had it a number of times.
- Long-term pain in your pelvis (chronic pelvic pain). This may be related to inflammation, scarring and adhesions from PID.
Prevention of PID
To prevent pelvic inflammatory disease (PID), you need to avoid getting a sexually transmitted infection (STI). Use safe sex contraception such as condoms.
- If your sexual partner is diagnosed with an STI or pelvic inflammatory disease, get tested too. And treated, if necessary.
- Don’t have sex with your partner until you’ve both finished your treatment for pelvic inflammatory disease or any STI.
- Regularly get tested for common STIs such as chlamydia.
- If you take antibiotics for pelvic inflammatory disease, make sure you finish the full course.
Worried about your Period health?
A personalised care plan for heavy, painful or irregular periods for those 18 and over. Now available.
Pelvic inflammatory disease is mainly caused by a sexually transmitted infection (STI). Anyone with an STI can pass on the infection. So, it’s important to use condoms to prevent passing on STIs. Some people get symptoms of STIs, but many don’t. So, if you think you could have caught an STI, get tested.
For more information, see our section on causes of pelvic inflammatory disease.
If you get pelvic inflammatory disease (PID), it can make an ectopic pregnancy more likely because of damage to your fallopian tubes from PID. This can make them narrower or block them completely. A fertilised egg can get stuck inside the tube and begin to grow and develop there. If you could be pregnant and have bleeding from your vagina or pain in your tummy, get medical help straightaway.
Pelvic inflammatory disease (PID) is almost always triggered or caused by a sexually transmitted infection (STI). It’s often an infection with chlamydia or gonorrhoea although other infections can also cause PID. The bacteria can move up from your vagina or cervix to your womb, fallopian tubes and ovaries, and cause PID.
For more information, see our section on causes of pelvic inflammatory disease.
You might not know you have pelvic inflammatory disease (PID) because symptoms can be very mild, or you might not have any symptoms. PID symptoms include pain in your tummy and an unusual vaginal discharge, which may smell. You may also feel pain when you have sex.
For more information, see our section on symptoms of pelvic inflammatory disease.
Antibiotics
Common vaginal infections
Female infertility
Getting pregnant (conceiving) often takes a while.
Did our Pelvic inflammatory disease information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Pelvic inflammatory disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2023
- Jennings LK, Krywko DM. Pelvic inflammatory disease. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 13 March 2023
- Pelvic inflammatory disease. BMJ Best Practice. bestpractice.bmj.com, last reviewed 7 July 2023
- Acute pelvic inflammatory disease. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, accessed 7 August 2023
- Gynaecological examination and history. Patient. patient.info, last updated 27 October 2021
- Chlamydia – uncomplicated genital. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2022
- Ectopic pregnancy. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised in February 2023
- United Kingdom national guideline for the management of pelvic inflammatory disease. British Association for Sexual Health and HIV. www.bashhguidelines.org, updated 2019
- Pelvic inflammatory disease. Medscape. emedicine.medscape.com, updated 16 August 2021
- Pelvic inflammatory disease. BMJ Best Practice. bestpractice.bmj.com, last reviewed 7 July 2023
- Sexually transmitted infections. Patient. patient.info, last updated 1 April 2022
- Ectopic pregnancy. BMJ Best Practice. bestpractice.bmj.com, last reviewed 7 July 2023
- Rachael Mayfield-Blake, Freelance Health Editor



