Employee resources for workers with cancer
Resources for your team
It's important to give your team the right support when they need it. That's where our resources can help.
Cancer prevention and awareness
Understand different cancers and get support if you or your employee has a diagnosis. Plus, find information on common symptoms and treatment options.
Helping children understand cancer
We've worked with specialists and families affected by cancer to create helpful guides. They explain what cancer is and look at the different types of treatments.
How to check for moles
We understand that knowing what changes to look out for can be hard. That's why we created our helpful guide so your employees can feel more confident checking their skin at home.
Cancer: your questions answered
Rita Trewartha, head of clinical services for Bupa UK and nurse with over 40 years experience, is here to answer your questions on cancer.
Transcript
Who are you?
Hi, I am Rita Trewartha
and I'm head of clinical services for Bupa UK Insurance.
I'm a nurse with over 40 years
experience, come and ask me about cancer.
What is cancer?
Cancer is essentially a group of abnormal cells.
So it starts in the cells in our bodies.
I try to explain it
that the cells are like tiny little building blocks
that make up our organs and tissues throughout our bodies
and for them to grow and divide
they get signals to do that.
And those signals also tell them when to stop growing
and dividing and to die because they're no use anymore.
But sometimes also those signals can go wrong
and the cell becomes abnormal.
And those abnormal cells may also keep dividing
and dividing more
and developing into essentially forming a lump.
Now, often you'll hear lumps referred to as tumours.
Now tumours aren't necessarily cancers, not all lumps,
not all tumours are cancers.
The way that we find out the difference is
by taking a biopsy or a small sample of cells from that lump
or that tumour to determine
what it's made up of, essentially.
So the tumour or the lump might not be cancer,
and that would be called a benign tumour.
It can still grow, but it doesn't spread anywhere else in
the body and it only causes problems
and needs treatment if it's pressing on a structure
or something nearby, a muscle or an organ.
If it's not doing that, it will live there quite happily
and not cause any harm whatsoever.
A tumour that is cancer is called a malignant tumour,
and that can grow into nearby tissues,
and that is called a primary cancer site.
But also what it can do is travel to other parts
of the body, and it can do that through the blood
or the lymphatic system in the body.
And if it does that,
then it can settle deposits elsewhere in the body,
which can form other lumps or tumours that can grow.
And that's called a metastatic cancer.
So a secondary cancer to the primary site,
but all part of the same cancer really.
I suppose the other thing to also mention is
that cancer can form in the blood cells or the bone marrow,
and that develops into what we call
as a group blood cancers.
So one of those that you might have heard
of quite frequently is leukaemia.
So in essence,
actually cancer is a group of abnormal cells.
How common is cancer?
So one in two of us will be diagnosed
with cancer in our lifetimes with the highest lifetime risk
for females being for breast, lung, and bowel cancer
and for males being prostate, lung, and bowel cancer.
And we have seen an increase over recent years in cases
that are being identified, but that's
because we are much more aware now of the risks
and we are being screened more regularly
through our national programmes.
So we are catching cancers much earlier.
For the 10 most common cancer types, more than 70% with
of those cases in the UK have been attributable
to known risk factors, and that includes lung
and melanoma, skin cancer, which are 2
of the 5 most common cancer types in the UK.
What can cause cancer?
When we think about causes of cancer,
we can't really just think about one thing.
I think it's really important to understand
that right at the outset.
So it could be, for example,
that there's been an inherited cancer gene variant.
So that's something a person inherits from a parent.
Now that doesn't mean you've got cancer,
it doesn't guarantee you are going to get cancer,
but it might mean that if you had some abnormal cancer cells
that would develop more rapidly than it would
for somebody without that gene variant.
And if that gene variant was common within a family,
as in more than one person in that family,
or several people had that gene variant in that family,
that could mean a certain type of cancer was more common in
that family than you would see somewhere else in
the larger population.
And I suppose we always need to throw in age as something
that is an increase in risk in terms of cancer.
But when we are thinking about that inherited gene variant,
it's really important to understand
that it's less than 5% to 10%.
So that's less than 5 to 10 people in every 100
that will actually carry that gene variant.
So lifestyle factors such as smoking, being overweight
or obese, drinking alcohol above recommended levels,
over exposure to UV radiation from the sun,
those are the things that are much more likely
to influence you or me on a day-to-day basis.
How do I know if I am at risk of cancer?
So a person's risk of developing cancer depends on lots
of different factors, including age, genetics,
and external risk factors.
So those more associated with lifestyle.
Understanding your risk means, for example,
understanding if there is any family history,
but also what those external risk factors are
and actually how they apply to your life.
So as we know, smoking and overweight
and obesity are the primary preventable risk factors,
and 35% of all cancers
that's about 135,000 cases every year are preventable.
So you can start to better understand your risk.
I think other things that help us understand risk include,
for example, that lung, breast, bowel,
and melanoma skin cancers account for almost two thirds
of preventable cancer cases in the uk. Over exposure to UV,
so the sunshine
and substances at work, drinking alcohol to excess,
and too little dietary fibre.
Each of those could be responsible for 3% to 4%
of cancer cases in the UK.
And then there's some lesser known exposure risks.
So ionising radiation, x-rays,
or eating processed food that can account for about 1%
to 2% of cases.
And then even smaller than that, air pollution
or doing too little physical activity
could cause about 1% of cancers in the UK.
What are the main forms of cancer?
Currently in the UK, more than half
of new cancer cases in males is prostate,
lung, or bowel cancer.
And in females, half of new cases are either breast,
lung, or bowel cancer.
Can cancer be prevented?
So research shows that 35% approximately
of cancers are preventable.
And we know that smoking is the largest single preventable
cause of cancer in the UK each year,
and that's according to Cancer Research UK.
And we also know that being overweight
or obese is the second highest preventable cause of cancer.
So these are what I would refer to
as modifiable risk factors.
So something we can try to influence or do something about.
Not always easy, it doesn't mean we can't try.
So stopping smoking, maintaining
or achieving a healthy weight through diet
and exercise, following the recommended alcohol intake
guidelines and protecting ourselves from those potentially
harmful UV rays
by simple things using sunscreen and covering up.
So there's lots that we can do to contribute
to the prevention of cancer.
What percentage of cancers are preventable?
According to Cancer Research UK, over 35%
of cancers are preventable.
There's been a lot of research on this
and the World Health Organisation estimate that figure is
between 30% and 50% worldwide.
The main point to remember is managing your risk factors
and watching for changes in your body or any symptoms.
Can vaccines help to prevent cancer?
So there's an awful lot of research going on in this area
at the moment that's looking really, really positive.
But one development that there has been is the vaccine
for HPV, that's the human papilloma virus
that was identified a number of years ago as certain strains
of it being responsible for a significant amount
of cervical cancers in women.
The HPV vaccine has now been rolled out as part
of a school's programme to 11 and 13 year olds,
and that has had a significant impact in terms
of the prevention of cervical cancer.
Does genetic testing help to prevent cancer?
No, but it can help to identify if you are at greater risk
of developing cancer.
Genetic testing is a really complex area
and the results can sometimes be very
difficult to interpret.
I think I would always recommend getting some advice
before getting any testing,
and then use that healthcare professional advice
to help you interpret the results.
Does the risk of cancer increase as you age?
Sadly, yes, but it's still important
to keep a healthy lifestyle.
Half of cancers in the UK are prevalent
in the over seventies.
It doesn't mean that you will get cancer, so
therefore it's still important
to manage those lifestyle risk factors,
and also important to access any screening
that you are eligible for,
and also seek health professional advice if you've got any
symptoms at all.
How can I protect myself against cancer?
So firstly, make sure
that you access your cancer screening programmes
as you become eligible
or any other routine health checks that are available
to you, either through your GP surgery
or possibly even through work.
But most importantly,
protecting yourself is about understanding
what the risks are and checking if there is anything in your
lifestyle that you can do to modify those risks.
We know, for example, smoking and being overweight
or obese are the leading risk factors,
and 1 in 20 cancer cases are caused
by being overweight or obese.
And that research identifies approximately 35 million people
in the country at the moment are overweight or obese.
Now, that's measured on the body mass index scale,
and A BMI of over 25 is considered overweight or obese.
So that's something easy that you can check.
So depending on your circumstances, there could be lots
of things that you can do to reduce your risk
of getting cancer.
Can I get cancer more than once?
Sadly, yes, it could be a recurrence
or it could be something new.
Follow-ups are important
and recurrent cancer starts with cancer cells
that the first treatment didn't fully remove or destroy.
Now, this doesn't mean
that the treatment you received was wrong.
It just means that a small number of cancer cells
survived the treatment and were too small
to show up in follow-up tests over time.
These then grew into tumours
or cancer that your doctor can now detect.
Sometimes a new type
of cancer will occur in people
who've had a history of cancer.
When this happens, the new cancer is known
as a second primary cancer,
and the second primary cancer is different
from a recurrent cancer.
A recurrent cancer can be localised,
so literally in the same place as the original cancer,
or it can be regional,
and that means it's grown into lymph nodes
and tissues near to the original cancer.
Or it can be a distant recurrence,
and this means that the cancer has spread to organs
or tissues far from the original cancer.
It's called metastatic cancer or metastases.
I've had cancer before can I prevent it reoccurring?
You can minimise the risk of recurrence.
So if you are on ongoing treatment
because you're in remission, sticking to that treatment
and having your regular follow-ups
is really, really important.
If you are completely in remission,
but you have lifestyle factors that might pose a risk.
So overweight
and obesity, exposure to UV radiation, sunshine,
it's about managing the risk factors associated
with a recurrence of cancer.
What are the most common misconceptions about cancer?
So I think the most common one is that it won't happen
to me or my family because there's no history,
but I think we all know somebody
that's probably been affected, so that just isn't true.
And then there's other myths around mobile phones
and the non-ionising radiation from those and burnt foods
and eating burnt foods.
Again, there's definitely no known link at this moment in
time in relation to cancer, plastic containers
and bottles drinking from them,
putting your food in plastic bags.
There's no evidence that increases your risk of cancer.
The same in relation to artificial sweeteners
and the same in relation to stress and pesticides
and genetically modified food.
None of those things have an increased link to cancer.
How can I check whether I have any cancer symptoms?
If you know what's normal for you, it's much easier
to notice anything that changes. So instead
of regular self checks doing the same thing the same
time on a regular basis.
Just be aware of what's normal for you
and listen to your body,
and if something doesn't feel right, then you need to go
and get that checked from a health professional.
Go and speak to someone.
Listen to your body and speak to that health professional
because we know if you spot cancer at an early stage,
that does save lives.
Now a lot of people do talk about those regular checks,
but there's no evidence that that really helps.
So think about if we are talking about bowel cancer,
for example, changes in that bowel habit.
How often you go to the toilet can be an indicator
and a symptom, but it's normal for you.
So if you normally go to the toilet twice a day
and everything's the same as normal,
then you don't need to speak to anyone.
But if you start going much, much more regularly
or you can't go at all,
or the consistency is different, then that's the time to go
and get some advice.
We try not to be too prescriptive of
how long those symptoms should be there
before you seek advice,
because what's normal for you
isn't necessarily normal for me.
So listen to what your body's telling you
and get that professional advice, even if it's only
to put your mind at rest.
What symptoms should I look out for?
So there are lots and lots of different types of cancers,
which means there's lots
and lots of different types of symptoms.
So it's really not easy to give a list
and not all of those might resonate with you
or ring true for you anyway.
So some symptoms are going to be really obvious.
You are going to have a lump somewhere
that you haven't had before.
You can see a mole that's changed and is different,
but other symptoms might be more vague than that.
So you might be off your food, you might have lost weight
when you're not trying to lose weight,
you might be tired all the time and not know why that is.
There might not be a really good rationale for that.
So it really is very much about you feeling
or seeing something different for you, or as a friend
or family member, notice something different.
Then go and get that checked out with a health professional.
What can I do if I think I have cancer symptoms?
So the first thing for me is be brave and speak up.
As soon as you can. Go and see a healthcare professional.
If you've had symptoms, write it down so that you know
what you're saying to the GP.
If you can take a friend with you to help you remember,
if nothing else, whatever the doctor says to you,
that's really, really helpful
because you'll come out of that appointment
and you'll have forgotten everything
that anybody's said to you.
So fundamentally, the really, really important thing
that you really must do is if you think you've got symptoms,
go and get it checked out.
When should I seek professional advice about cancer?
Trust your instinct.
If something isn't normal for you,
if you think you've got symptoms, please go
and seek some professional advice.
If you're a Bupa customer, we have our direct acts
to cancer service so that you can phone us up
and we can give you a direct referral
to a consultant without consulting a gp,
or you can see a GP through our digital GP service,
and we also have our 24 hour Anytime Healthline manned
by nurses 24 hours a day, seven days a week.
Also, if you're invited to NHS screening appointments such
as mammogram or bowel cancer screening,
or for testicular checks,
please make sure you keep those appointments.
And do remember, just
because you've been screened, that doesn't mean
that you don't need
to get checked if you develop new symptoms in
between those screening times.
So if you get any new symptoms, even between your screening,
please also go and get those checked.
What should I do before going to the GP?
So gather your information,
get some support if you want somebody
to accompany you to your appointment.
Remember, the more detail you can share, the better it is,
but it's also not a test.
You don't have to diagnose yourself.
That's what the doctor's going to do.
And think of the questions that you want to ask.
Take your time and don't be afraid to say
that you don't understand when you get
the answers from the doctor.
Just because they've explained it once doesn't mean they
can't explain it again.
Check what happens next.
If the doctor suggests you need some tests
or investigations,
make sure you find out when they're likely to happen,
when you are likely to get the results.
And I think another important thing to do is
to check what you need to do.
If you are waiting for any investigations
to happen, who do you contact?
Who's best to follow up with?
Where can I go for helpful information about cancer?
So there are lots of trusted resources out there,
Bupa's own website, .co.uk, the McMillan website,
and also Cancer Research UK.
And of course, the NHS has got
loads and loads of information.
But please, please make sure you use one
of those trusted websites.
But if you've got some symptoms
that you are actually concerned about for you right now,
it's really important to speak to a health professional
and get the reassurance you need.
How do I access support through Bupa?
If you're a Bupa customer,
we have our direct access service where you can get straight
through to see a consultant without a GP referral.
If you already have a GP referral,
you can call our member services line.
We will assess your eligibility
and guide you to the most appropriate special.
Guidance and support from our experts
Our experts are joined by some familiar faces as they discuss signs and symptoms as well as tackling some well known misconceptions.
Inside Health:
Tackling testicular taboos
Chris Hughes, TV personality, chats with Bupa's Dr Naveen Puri about the signs and symptoms of testicular cancer, how to do a self check and what diagnosis and treatment options are available. They also answer some common myths about testicular health.
Sometimes life takes really unexpected turns, and I've always been passionate about talking men's health, and you don't know what's around the corner.
Back in 2018, I went on This Morning to undergo a live testicular examination to discuss the importance about men checking themselves and how to do that correctly.
It's really given me the drive to keep talking about this important topic.
It's around 95% curable if diagnosed early.
So today I'm joined by Dr. Naveen to unpack this important topic.
So Dr. Naveen, thank you very much for joining me.
Thank you for having me, Chris.
And welcome.
And we are in a changing room.
I think the important thing around this is the fact that you know, as men in changing rooms, in sport teams, we do a lot of talking, but it's not necessarily on the topics which are actually important within our lives.
You know, it's quite a stigmatised subject, talking about testicular, how we all shower together, as we know.
But I feel for like women, it's a lot easier to do.
They go down to the park, they go out for drinks, and they'll talk about those important subjects.
But as men, we don't necessarily do that.
Yeah, I'd fully agree Chris.
I think it's one of those rare places that men are actually vulnerable, isn't it?
As you say, we shower together, we talk together.
This is like one place we can truly be open.
So let's see if we can replicate some of that banter, and.
Absolutely.
And well, the first thing, checking your testicles.
It's the easiest thing to do in the world.
Is it not?
It really is.
And that would be easy for me to say as a doctor, but honestly speaking, a testicle is really a small structure to check.
It takes literally seconds.
And if we're asking you to check both your testicles once a month, which is the frequency we recommend, it shouldn't take very long at all.
And we've got some props.
We do indeed.
So out comes the satsuma.
Right.
Show me exactly how you should do this correctly.
All right.
So a satsuma, as most men will know, is much bigger than their actual testicle is, but this is a little bigger just so we can demonstrate to our audience how to do an examination.
The first thing is you want to stabilise your testicles.
So if you take the finger and thumb of one hand and just hold your testicle or satsuma like this.
Yeah.
Your other hand is free, and you've got your finger and thumb on that hand, and all you want to do is just make sure you run around the entire smooth surface to make sure there's no lump on there.
Your fingers have hundreds of nerve endings, in fact millions of nerve endings, so that if there was a lump on there, you'd pick it up really easily.
So stabilising the testicle, all you want to do is take your finger and thumb and just run them entirely around your testicle to make sure it's smooth, from one end down to the other.
So maybe start at the top and work down, or start at the side and work to the other side, whichever is easier for you.
Is that easier to do when you've, I know when we have a bath as men, everything relaxes.
Yeah.
So it gives you a more kind of, Spot on.
full on approach to it, I guess.
Yeah, absolutely.
That's a great tip.
So when you have a bath or a shower, the testicle actually falls down from the body because the testicle has to be slightly cooler than the body temperature.
So having a bath or a shower, or even just some kind of workout, when you're hot and warm can lower the testicles and make it much easier to examine your testicle as well.
I like you just mentioned that you're touching it.
So we are literally looking for any kind of lump or anything what doesn't feel natural.
Yeah, absolutely.
So as I said, it should be completely smooth.
Just like that satsuma surface is.
If there was a lump or a projection on this, so let's take, for example, a pea.
If there was a pea stuck on that or a lentil stuck on that, hopefully, your finger would pick that up quite easily.
But you have to be feeling to know it's there.
The body gives you no warning signs, so unless you're feeling, you're not got to know one is present.
And that is essentially what happened with my brother.
So I did the live examination that day.
I went home, I went to bed as you do, and three o'clock in the morning, he knocks on my door.
And I did say to him, I was like, Ben, what are you, what are you doing?
It's three in the morning.
He goes, I think I've got a lump on my testicle.
I said, well I'm not getting up at three o'clock to check it right now.
It can wait until the morning.
Yeah.
And then he showed me in the morning and obviously, there was a lump there, which he then went and got diagnosed.
But what would you recommend for people if they found a lump on their testicle?
How would you then go about the secondary approach to that?
Yeah, well thank you for sharing your story, Chris.
And I think your brother took exactly the right approach in checking himself, and well done for having done so.
What I'd say to anyone that feels a lump is don't be alarmed.
There can be many things that can cause a lump, but we have to be concerned to rule out a possible cancer.
In young men in particular, there are very few things that cause a lump.
And so if you've got one, let a doctor do the work for you.
And so you need to take yourself to the doctor so that they can do the next stage of investigation by referring you on to a specialist.
And I think what you just touched on there is very important.
I mean, a lot of people don't necessarily want to put themselves through the anxiety of going and getting themselves checked out.
They might kind of, I think a very common thing we do as men is like bypass the situation.
Yeah.
And put it to one side and think, okay, there's a slim chance it might be cancer, so I'm okay, I can deal with that.
Yeah.
Because with testicular cancer, it is a pain-free situation, isn't it?
It's not something which is physically got to give you pain or any feeling to kind of alert you in that respect.
Yeah, absolutely.
And I feel like men, we can ignore that.
We can put that to one side, and that's not a good approach is it?
Yeah, no, spot on.
I mean, I think as men, we tend to bury our heads in the sand, don't we?
And unless there's a symptom such as pain or a rash or something which you can see or feel, you're not inclined to want to go and see a doctor.
I'd say a couple of things.
One is that testicular cancer actually affects younger men more than it affects older men.
So men that are the age that you're in Chris, and your brother, will certainly be affected more than say the men in my age group.
And so it's very important that you do recognise that.
The second thing to say is that when you go to a doctor, I know for a patient or for a gentleman like your brother, it's the most daunting thing.
But for a doctor, we probably see several a week actually.
And it really is just run of the mill, another gentleman with a testicular lump, let's refer onwards to a specialist.
We'll do our best to make you feel as comfortable as possible.
But it is important you get through the door, because if you don't, no help is available to you.
Yeah, and I know why we are in a rugby change room, It's quite a fitting setting.
'Cause I was chatting to Gareth Thomas about this similar situation when we were doing some filming together, and he was essentially saying he doesn't want to, or he didn't want to check himself, because he feels like what he doesn't know can't hurt him.
Right?
Yeah.
And I'm sure his approach would've changed in that respect, but the way I see that, I feel like if you do check yourself, and you don't find a lump, Yeah.
or if you do find a lump, and then you get it cleared as being fine, you can continue to check yourself every month, which you'd probably recommend.
You can tell us a timeframe in a minute.
But if you check yourself then, going on every month after that, it gives you that security in your head that if you then do find something afterwards, you've caught it early and at a good stage.
Yeah.
That is spot on too.
So in terms of frequency, I would say do a check once every month.
A good time as you've recommended is when you're just out of a bath or a shower 'cause the testicles are slightly lower in the body.
Even after a workout, you're a lot warmer.
And so doing it then is a good time as well.
It takes literally seconds.
So if you, the first time you do it, you may want to take a bit longer just to, you know, sort of get a real feel for how you do it.
I'd also say to men, get to know your testicles.
We always tell our female patients to get to know their breasts when they do a breast exam, and the same applies to us as men as well.
Get to know your testicle, get to know what normal for you feels like.
And if you do it month on month on month, if there ever then is a change, you'll think, oh, hang on, that's not normal for me.
Let me go and take myself to a doctor.
And you can see it much clearly.
Yeah, absolutely.
Whereas if the first time you do a check, like your brother perhaps, and that's the first time you pick up a lump, you may then wake up your sibling at three o'clock like your brother did with you and you know, raise the alarm, which is absolutely fine to do, but you may also just think that's normal, and that would be really disastrous.
But it's literally 10, 15 seconds, that's all it is.
It takes no time to check yourself.
If you do that 10, 15 seconds on each testicle once a month, that's 30 seconds of your life.
Yeah.
Thank you for that.
Which could save your life.
Yeah, it really isn't that big an ask, is it?
But yeah, as long as you make it a routine, make it a regular thing for yourself, that's all we're asking you to do.
So why do we feel embarrassed about it?
What is the problem?
You know, it's hard to pin down, Chris.
I mean, there's a couple of things that I speak to mine, based on the patients that I've seen.
I think one of the biggest things is an embarrassment about seeing a doctor and getting naked in front of them.
But as I've said, doctors see naked people all the time.
It's a part of our routine.
We'll do our best to make you feel as comfortable as possible and just talk you through the process so you know exactly what's going on.
I think another thing is the fear of the unknown.
I think some patients come to us and recognise that they may have something wrong but don't want to know what's got to happen next.
For some men, being medicalised can be quite scary.
Things like the fear of impotence and not being able to get erections, not being able to have children which are not the case, by the way, can often cloud their their ability to come and see us as well.
So there's many myths and wives' tales out there as to why patients don't see doctors.
But honestly, it's always the right thing to do.
So please do bring yourself to a doctor whenever you need to.
I think one important thing you said there, Dr.
Naveen, is you've seen everything as a doctor, and that is the thing for men to understand.
Yeah.
Especially people who want to go and get something looked at.
There's nothing you haven't seen.
So nothing's new to you guys.
So that embarrassment factor shouldn't really be there.
Should it?
Yeah, absolutely.
And I think it's important that we emphasise that.
For a doctor, we see these things day in, day out.
And really, a good doctor will make you feel comfortable around that.
We'll recognise the very brave step you've taken to come and see us.
But it's then for us to make you feel comfortable and take the next steps for you.
And in a very basic form, what is that next step?
So if you have got a lump, without x-ray vision, we can't tell whether it is a serious lump or a non-serious one.
So what we'll do is refer you to a specialist, and they'll do what's called an ultrasound scan.
This kind scan that pregnant women have over their tummy.
So you'll have some jelly applied to your scrotal sac, or your ball bag, we'll apply a probe over it, much like a deodorant roll on.
And that will give us a 3D image of your testicle.
Completely painless, takes literally minutes to do, and it gives us an image of what's going on, and we can then decide next steps from there.
And then after that, what would be the next stages of a cancer diagnosis?
Yeah, great question.
So as with any cancer, we then need to do something called staging to see how far the cancer has spread.
And the great thing with the testicular cancer is that if it's caught early, it is completely curable.
All cancers start off being contained essentially.
They're confined to a small area.
And unless they've spread elsewhere, all we have to do is simply remove that cancer, and you are completely cured.
Now, testicular cancer grows relatively slowly in the first few months, before it gets a lot faster and starts to spread elsewhere.
So if we catch it in the first few months of it being there, you are really in a much better position than if it's a bit more further afield.
I think that's why it's important to remember that 95% curable.
Yeah.
Is a great reason in itself just to get yourself checked.
Yeah, absolutely.
And if you consider a testicular cancer, it's so easy to pick up as well.
All you have to do is feel your balls through your testicular sac, and it takes, as we've said, about 30 seconds to do every month.
It really is a very easy one to pick up if you consider that other cancers that occur within the body can be much harder to pick up.
We really have no excuse for not detecting and then treating and curing testicular cancer.
is not a long time to put aside for what could save your life essentially.
Absolutely.
I mean, when you consider how much time we spend on social media or watching TV or even an advert between one of our favourite programmes, that's longer than 30 seconds.
Exactly.
If we can do all those things, there's no reason why we can't check ourselves as well.
A hundred percent.
So what things can we do to reduce our chances of getting testicular cancer?
Are there any lifestyle factors we can change?
Great question, Chris.
I mean, a lot of patients ask me what can I do to reduce my risk?
Because with the awareness, people are now looking to control their risk as well.
What I will say is that with all cancers, so let's speak generally, first of all, we know that there are certain things that certainly increase your risk of a cancer.
Things like being a smoker, things like drinking too much, things like being overweight and not exercising enough.
Those lifestyle factors certainly are cancer causing across the board.
I will also say, though, that testicular cancer, because it occurs relatively early in life, means that you've not always had enough exposure to the harms of cigarette smoking or drinking too much or other things that could cause a cancer.
And sometimes it is just bad luck that your testicles happen to develop a cancer in the circumstances that they do.
We know that some people have a genetic predisposition to that.
So sometimes you will hear about certain relatives in a family being affected, or certain relatives being affected when somebody else is diagnosed.
And so aside from being healthy and just being vigilant to the cancer being there by doing a self-examination, there probably isn't much else that I'd recommend people do at this stage.
Obviously, a subject I talk loads about, as well is my brother.
He was the one who had testicular cancer.
My cousin had it as well.
His cancer becomes secondary of the abdomen, but thankfully it was fully cured as well.
So again, it showcases the fact that testicular cancer is a hugely curable cancer.
Yeah.
Is it something which runs in the family?
Is it something that people should worry about in the family?
Is it genetically connected?
Yeah, let me be really honest with you.
I think medicine moves really, really fast, and we are constantly discovering new things about not just cancers, but all sorts of conditions.
But speaking about cancer in particular, there is a real knowledge base now around which cancers do have a very strong genetic link.
So there are certain kinds of breast cancer or bowel cancers that are very genetically driven.
We haven't discovered a one-off gene that causes testicular cancer, but we can't deny that there are clusters of testicular cancer that occur in families, and I think your family is one example, in point, with around that.
So we do know that there is some element of heredity in that equation.
What I'd say is that if you have got a first degree relative such as a brother or a father affected by testicular cancer, it does raise your risk quite considerably.
Okay.
If you've also got a second degree relative like a cousin, that also raises your risk, we're not sure by how much, but certainly does raise that concern there.
So I'd say for all men to be checking themselves regularly is important, but especially those men who have relatives who are affected as well.
Because if they've been affected, you may have a similar gene or genetic makeup which makes you prone to it as well.
Amazing, Dr.
Naveen.
That is very good advice for any man wanting to check themselves on how to do it correctly.
And if you find something, do something.
Perfect.
Simple as that.
Absolutely.
Though I think you've hit the nail on the head, Chris.
Being proactive is the most important thing.
And as long as you're doing that, you're good to go.
(upbeat music)
The Doctor Will Hear You Now Podcast:
Bowel Cancer
Dr Zoe Williams is joined by the incredible, Charlene White. Charlene discusses her experience of bowel cancer, including the diagnosis and sad passing of her mother. They are also joined by Dr Petra Simic, Medical Director for Bupa Health Clinics, to bring her own expertise to this subject matter.
(lively music) Now, today's topic is the only episode in this series where we're mentioning the big C.
Today we're got to be discussing bowel cancer.
And bowel cancer is one of the most common cancers in the UK.
It actually affects one in 15 men and one in 18 women.
But despite that, there's still a reluctance amongst many people to talk about their bowels or even look at their own poo.
So it's really important that we have this conversation today.
And one person who devastatingly was diagnosed and died from bowel cancer was the mother of today's guest.
Charlene White is a staple of broadcasting here in the UK.
She's a journalist, news presenter, an all round household name.
But Charlene was just 21 when her mum, Dorette, sadly passed away from bowel cancer.
So I'm so grateful to you, Charlene for coming to have a chat with me about it today.
Thanks for having me, Zoe.
The first question I'd like to ask you is what's the one thing you should never say to somebody whose life has been affected by bowel cancer?
Ew.
Because a lot of people find the whole discussion around bowels, around poo, despite the fact that every single one of us has to have a poo at some point during the day, people do find it a bit icky.
And I would say never sort of recoil when someone talks to you about the fact that they've been diagnosed with bowel cancer.
Don't recoil when someone even has a conversation about it.
I think for some reason, and I can't quite put my finger on it, people find it really disgusting to be talking about bowel movements when there's nothing disgusting about it at all.
It's healthy.
There's a reason why we do it.
And the more uncomfortable we are with that conversation, the more likely we are to ignore very obvious signs when something's wrong.
You're absolutely right, aren't you?
You know, it's a bodily function.
They're our bodies.
We own them.
But I do experience that all the time.
I'll have patients and they'll have symptoms, bowel symptoms, and I'll say to them, you know, have you noticed any change in your poo?
Is it a different colour?
Has it been looser?
And like you say, they'll recoil and go, "Ew.
Oh, I don't look at my poo.
" Why not?
It's yours.
It's so strange.
And considering the numbers, the high numbers of people that are affected by bowel cancer, it shouldn't be that situation.
I mean obviously there are loads of other signs as well, and unexplained weight loss being one of them, a change in appetite being another one of them.
There are so many different signs that people seem to ignore or seem to not want to go and talk to a doctor about when there's no reason for you to die from bowel cancer because if you have an early diagnosis, you're able to live a long and fruitful life.
It's when you get that late diagnosis that issues arise.
And I sort of say to people, before you flush the toilet, instinctively, you look in the toilet before you flush the toilet.
So just look in the toilet and if something looks different, something has changed, there's no reason why you cannot pick up that phone and talk to your doctor about it.
Yeah, and the first step, as with everything, is getting to know your normal.
So for people who've avoided looking at their own poo, start looking at it.
Get to know what it looks like, you know, and it does fluctuate from time to time.
It can be a bit looser, you know, we can get a bit constipated, but if people have a sustained change that seems abnormal for them, please don't leave it.
Just get it checked out.
Yeah, and I know it can be quite a scary thought to go in and see your doctor, to go in and see you and sit down and start talking about your poo.
Yes, it might seem really weird and it might make you feel a bit uncomfortable, but it could save your life.
So who cares if it's an uncomfortable conversation?
You have to take control of your own life and be aware of your own body because that first step is on you.
Your doctor doesn't know your body instinctively when you walk into a room.
You know your body.
So that first step is very much on you.
The rest of it is where you guys come in.
But that first step is very much about the individual and we have to get over the fact that we might feel a little bit weird talking about it.
Yeah, because as doctors, you know, we don't feel weird.
That's a normal part of our job.
We're not phased by anything like that at all.
We're very comfortable to talk about anybody's poo.
(both chuckling) So this conversation today, we're got to talk about your mum, Dorette, who sadly passed away from bowel cancer.
First of all, let's hear a little bit about her.
Paint a picture of your mum for us.
She was brilliant.
She was very loving.
She had three kids.
She worked very hard.
She was a strong believer in education.
So we all had to do well with education.
But she let us be very free to like extracurricular stuff.
She came from a big family.
She was an immigrant here.
She went to secondary school here, which very much controlled or it was the start point for her in terms of how she chose to educate us because of her experience and education here as an immigrant from Jamaica.
She was very loving.
She was very nurturing and she liked looking out for people.
My family always say that our house was the centre of everything for both sides of our family because our doors were always open and that had a lot to do with her.
Yeah, and you grew up in Southeast London?
Yeah, in Southeast London in Lewisham.
So we say I'm a Blue Borough kid, very proudly say.
And we were surrounded.
.
.
I was in a very Jamaican household, surrounded by family, surrounded by friends.
Could be a very strict household because my mom grew up in the church, but also let us make our own decisions once we reached our mid-teens as to whether we continued that.
But yeah, we were surrounded by, you know, getting up on a Saturday morning and going to Lewisham market and buying our Jamaican food to cook for dinner that week and that that weekend.
As a parent now, I have no idea how my mom and dad juggled everything they did 'cause they worked sort of five, six jobs between them in order to send us to school whilst also being parents, whilst also making sure we're all right.
My mom also studied as well so she could get her degree in social work.
You know, they were busy.
They were a busy couple.
I heard you speaking about this on another podcast and you were saying, you know, your mum would get up in the morning and she'd prepare the food and she'd sort of put it on a slow cook so that then, you know, your dad would be the one who would pick you up from school.
So the food was there and he could give you the food.
Then he'd go back out to the work when your mom got home and they really worked hard.
Yeah.
I mean, you'll understand the juggle.
There was all this love and-- Yeah, I mean, sort of, I grew up in a household where, yes, my dad would take over the other half of cooking and he would prepare dinner for us.
And then my mom would get back in from work at half past five.
And then he'd go back out to work and start at six in the evening having gone to his first job at six o'clock that morning.
And then at six o'clock that evening, he'd go to the second job and then he'd get home at just after 10 o'clock at night.
And then get up the following morning, rinse and repeat.
It'd be exactly the same thing.
A juggle.
Yeah, and I remember when, because pasta wasn't a thing when we were growing up.
It started later on in life.
Pasta became popular here.
And I say that because it was my overriding memory of my dad cooking pasta for the first time.
He cooked it like rice and absolutely burnt the pot to cinders 'cause he thought you had to boil all the water out.
And it was disgusting.
But, you know, it was a learning process for him.
So he was very much able to cook in our house.
So sort of being around dads and being around men who didn't do that, I always found quite strange 'cause my parents wouldn't have been able to do what they do if it wasn't 50-50.
Yeah, I think we think of it as kind of a modern thing, don't we now?
Both adults in the household, if there are two adults in the household, work and juggle, but actually, your parents were very much living that.
Yeah, and it's also a very modern thing where there's a lot of angst regarding both parents working.
But that was my normal, both of them going out and working whilst also parenting.
That was my normal.
And I don't feel like I missed out on anything.
So do you remember the point at which you first heard your mom's diagnosis?
Yeah, we were in the kitchen cooking Sunday dinner.
And I can't remember if we'd been to church that day.
Probably 'cause once she was diagnosed, she then started going back to church on a much more regular basis.
So we were cooking Sunday dinner and it was like literally in the middle of probably me washing the rice or something or soaking the peas for the rice and peas.
'Cause for people that don't know, a Jamaican Sunday dinner has Yorkshire puddings, but also rice and peas.
Yes.
Rice and peas.
And roast potatoes.
All of it.
It has everything.
And she just sort of very nonchalantly mentioned it in the general conversation that we were having that day as we were cooking.
And she said that she'd been diagnosed with cancer, that she had bowel cancer, but that she was got to be fine.
That she was got to start doing some treatment and it might make her tired but essentially, she was got to be fine and there was nothing to worry about.
And she just needs to let me know because things were got to be slightly different with the school-work routine.
And I was 16 at the time and she said, "But I'm got to be fine.
This stuff is happening and the treatment is happening and you know, I've been to the doctors, they've talked me through it, but it'll be fine.
" I was like, "All right, okay.
" And then we just went back to cooking again.
Now that I'm a parent, I realise that she probably did that conversation over and over and over in her head to find the right way to say it to me 'cause I was the eldest, the right way to say it to me so I didn't panic.
So I don't remember, you know, running off in floods of tears because she didn't make it sound awful.
She made it sound like it was a perfectly normal thing and we just carried on cooking and then we ate and it was fine.
So if you were just 16, how old were your brother and sister?
There's five years between me and my sister.
So she was 11 and there's 13 years between me and my brother.
So he was three.
Wow.
Yeah, gosh.
I think, and as you say, you know, at the time, you were only a child, but now as a parent it must have been so difficult for her to even contemplate having that conversation.
When I think of three, my daughter is three, and it's really hard for me because I can't imagine the thought of having to leave them when she's just three.
I mean, my daughter and I are very similar, very similar people.
She's very different to my brother.
My brother was very much the youngest child and a lot quieter because he had two older sisters who made more than enough noise in the house.
So he was definitely the quieter of the three of us.
And I can't imagine as a parent, as a mum, the thought of getting that diagnosis and she was a late diagnosis and knowing that there was a chance that she wouldn't see him grow up.
As a parent now, I can't imagine emotionally what that can do to someone.
So how did things progress from there?
Because she lived for quite a while with the illness, didn't she?
Yeah, so the average at that point was four years.
So she did just over almost five years.
So in between four or five years.
So she was about average at that point in time.
So she was diagnosed in 1996.
So she was in and out doing treatments, chemotherapy, radiotherapy at different points.
Her big thing obviously was really, really worried about losing her hair, which is the same for everybody that gets a diagnosis.
I always think it's slightly more pronounced within Black women because you were taught throughout your entire life that your hair is your beauty.
So you're under a lot of pressure to keep your hair looking nice and shiny and healthy.
We are defined by our hair as Black women.
So she was really scared about that.
So she always considered herself one of the lucky ones 'cause she didn't lose her hair through her treatment.
She would do her treatment in the morning and go to work.
There'd be moments where she would have her treatment where she had to be hospitalised for her treatment.
I don't know how my dad did it to be honest.
We have a wonderful family who were there every step of the way.
But there'd be weeks where she would be hospitalised for treatment, and my overriding memory is taking our portable tele out of their room, sticking it in the car, driving it to Greenwich Hospital and putting it at the end of the bed on the wheelie table that you have and sticking various coat hangers in it to get signal so that she could watch "Coronation Street" and "EastEnders.
" And we would lie on the bed and do our homework.
So she'd help us with our homework and that was normal for us.
But normal families didn't have to do that.
They'd be at home and doing that stuff.
But my normal was sort of lying in a hospital bed in the middle of my mom's treatment.
There's something about children, isn't there?
That children are very, very resilient and I think able to, even though a very abnormal situation, scenario like that, for most families see that as their normal and almost have some kind of, I don't know, still have joy and happiness and love and all those precious moments.
You still absorbed that, but you had to take on a lot of responsibilities then did you as the eldest?
Yeah.
And I also see that as sort of being normal.
I don't think I really got my head around those responsibilities probably until my mid-20s.
And I'd look back and just sort of think it really wasn't very fair.
But at the time, I didn't really realise that.
So I was doing a lot of parents' evenings with my dad.
What I realised in my 20s is my mom, essentially from 16, when she got that diagnosis, it was a very conscious decision for them to start giving me more responsibility because they didn't know how long she was got to be around for.
So there was always a schedule so they would know when I'd be at work.
I made the decision not to go away for uni.
I stayed at home because my responsibilities were at home.
So I could still do the school drop offs and stuff.
I could still do the parents' evenings.
My school allowed me to not make morning assembly, no bad thing.
So I didn't have to do morning assembly in sixth form because I'd be dropping my brother to school first and to nursery first at his school.
And then I would go into to school myself and then my dad would do the pickups.
I would come home from school, I would help with homework and such, and I would help with bedtime.
So I was doing that from 16 like many families do across the country.
And I was the enforcer.
So if my brother was naughty, my dad would always be like, "Don't make me call your sister.
" Really?
And I'd be the one doing the telling off.
And I was the one that was very, I was very tough with them.
And they took that from you, did they?
Even though you were their sister?
Oh yeah, yeah.
They took your discipline.
Yeah, I can still do a very, very, very good telling off of my brother and sister even at this older age.
I can still very much do that because although they are my siblings, I've always had, from my mid-teens, a very different relationship with them as a result.
And the reason why my mom did that is they, I guess is because she still wanted them to have a mother figure in their life if at some point she wasn't got to be here.
And I think they did that well and it seemed seamless to me.
It seemed really normal for me to take on more responsibility.
It was only sort of in my mid-20s that I'd look back and think, you know, everyone else didn't have to put their work schedule up on the wall.
Everyone else wasn't making sure that the shopping was done.
Every Thursday night was shopping night.
I'd go to Sainsbury's and do the weekly shop.
No one else had to do that.
But that's the responsibility that I had.
But they did make it very seamless for me, which I'm really thankful for.
Yeah, yeah.
At what point did you realise that you were got to lose your mom?
Can you remember that time?
Yeah, so they sort of sent her home for the final time at 21.
So it was the April and I turned 22 that June and I think it was about four weeks before she died that they had said to her that there was no more that they could do for her.
And anybody who's done cancer treatment or watched someone have cancer treatment, they know there's a change in the skin.
So any time she had treatment, her tongue would get black spots on her tongue and her skin, she'd have darker patches on her skin.
So I can tell now in family pictures, the pictures where she was having treatment, the pictures where she was in remission, I can tell because of her skin.
And her skin had been dark for a while and it hadn't gotten better and she didn't have as much energy.
And then she came home and she sort of said, you know, "There isn't a lot more that they can do so, you know, I'm just got to stay home now.
" And I realise now as an adult that decision was made because she didn't want us to have to go to a hospice and she wanted to make the process as normal as you can make that process.
So she came home to die essentially.
And it's got to sound really weird, but it was really beautiful moment in time because anybody that has a Caribbean family will know that it's kind of like people just descend.
So for four weeks, our house was packed full of people.
There're various aunties.
There was a constant flow of food in the house.
None of us ever had to cook 'cause there was like constantly food in the house.
My mom had clearly had a conversation with my aunt in Jamaica, my auntie Annette, to say that the moment at which there is nothing more they can do, she was to fly over and essentially be in the house with us.
So she'd help with that transition.
So she arrived from Jamaica and lived with us for quite a few months and was there to help.
My uncle set up a dominoes room in our garage with a Calor Gas heater, a little table to play dominoes on.
There was a constant flow of white rum and Appleton in there.
And you'd constantly hear, there was a.
.
.
They had music in there and stuff and in the house, there was a constant flow of church brothers and sisters that were coming to pray with my mum.
The house was packed, my friends were there constantly day and night, my friends were there and they wouldn't leave till late at night until I was going to bed.
There was always someone there in the house.
We were never there by ourselves, which also helped that transition because it made it a really beautiful time as well.
Yeah, yeah, so you can look back actually and whilst it was the most devastating thing was happening, you were actually having a really, I guess, it was a really enriched part of your life because, well, Jamaica came to Britain It really was, and you know, my brother obviously was still really young, so his best friend Charlie, his parents had been amazing with him.
And they'd taken him away quite a lot over school holidays.
And during that period, they would, you know, rock up to take him to school, would drop him back sometimes, take him to their house to have dinner and then take him back, drop him off to rugby training, all of that stuff.
It was like we had an army.
Yeah, I was got to say it's like a village, but it was more like an army.
It was an army of people and of friends and family and acquaintances and work colleagues that they had built up over years who showed up.
They all showed up and we were really lucky to have that.
It's giving me goosebumps that hearing about it.
So then the household was really, really busy, everybody was there to help, there was all this food.
And then when your mom did sadly pass away, did they stay?
Was that a quiet time?
How was that?
No, well, then that's when the Caribbean kicks in again because after death, the house, the rules are, the cultural rules are the house is full until the funeral and the days after the funeral and the night that she passed, again, we'd had a house full and we had Macmillan nurses that were helping overnight so my dad could get some rest.
So my dad would be in my brother's room, he'd set up a camp in my brother's room and the Macmillan nurse would stay overnight.
The Macmillan nurses are angels.
And my friend Leon, as he had done every single night, he was at the house watching telly with me.
And he must have left about 11 o'clock, I think.
And he only lived around the corner.
So he wandered around the corner and as I was going up the stairs, the Macmillan nurse came out my mom's room and just went, "It's time.
" So I then went and woke up my dad and woke up my brother and my sister 'cause me and my sister's room were in the loft.
So I woke my sister up and then we came downstairs to say goodbye.
I then called Leon 'cause I knew he was awake.
And I told him it was time.
And then he then clearly, they clearly had like a system in place.
My best friend down had already told me.
He had a conversation with his boss to say that something may well happen where he won't be able to come into work for a few days.
So I didn't know, unbeknownst to me, Leon had done a call of everybody.
My aunt had done a call of everybody and before I knew it, our house was full again.
And my friends were there and the doctor came and obviously, the car, van that they take the bodies away, that had all been organised and like the van was there.
I was very much, my friends were making sure my sister was fine.
I was making sure my brother was okay.
And then suddenly, we just like had a house full again.
And I remember leaving my friends downstairs in the living room.
I was like, I'm just got to take Joshua up to bed.
So I took Josh up to bed with me and I obviously fell asleep with him 'cause I was sort of stroking his head and making sure he was fine.
And then I woke up in the morning and realised, yeah, that did happen last night.
And I came downstairs and my friends were all camped out in the living room.
They'd gone into my sister's room 'cause that's where the airing cupboard where they'd found all the blankets and the pillows and the sheets and everything.
And they'd slept the entire night in the living room, which I will forever be thankful for them.
Sorry, I always get quite upset at bit.
Sorry.
You okay?
And they stayed and they stayed for days.
And I'm forever thankful for them for that.
And everybody else really 'cause our house was then full and it was a horrible, horrible situation.
But then there's joy that comes from that as well.
And it was really joyful because again, everyone descends.
And there's food and there's music.
And there's the nine night.
And the nine night, for those that don't know, it's the ninth night after someone dies in Jamaican families, you have a celebration of life.
So it goes on all night till the sun comes up and there's music and there's food and there's prayer, but there's dancing and there's dominoes and there's everything.
And our house was packed full of people on the nine night.
And then you have the funeral, which is a celebration of life again a few days after that.
So I know it sounds really bizarre and I know I've just like burst into tears, but because I'm really thankful, because it's so different from say death within British culture or English culture 'cause Irish are very, and Northern Ireland, Ireland, they do it in a very similar way.
It's very much a celebration.
It's not quiet, it's not mournful.
It's a celebration and it's loud and it's raucous and it's beautiful.
And I'm very proud that we have that in Jamaican culture because it makes that memory not a sad memory.
It makes that memory a really beautiful one.
Honestly, thank you so much for sharing that with us because you know, I'm dual heritage.
My dad's Jamaican.
My mum was white and I lost my mum and we didn't have that.
And it's actually everything around her death was quite sad and not balanced by the other side, the joy, the community, the friendship, the people showing up, the love, like the abundance of love that you felt.
And I think thank you so much for sharing.
I was feeling a little bit of what you felt and I think there's a tissue for you there.
Oh, thank you.
I've probably got makeup running down my face.
I should have worn waterproof mascara.
You look beautiful and luckily, these lights are fantastic.
What I wanted to ask you about is do you think that in recent years, the conversation and I guess the tone of conversation around bowel cancer and bowels in general is changing.
I mean, we've had some very brave, wonderful high profile people, Adele Roberts and obviously, Dame Deborah, who sadly died last year, who have campaigned and done so much to get us normalising conversations about bowels and poo.
How much do you feel that it's changed in recent years?
I think there has been a shift and Deb's was brilliant with that and I know that more people have gone to be tested as a result of her campaign, which is brilliant.
And I don't want that momentum to ease off at all.
I feel like, yes, there are more people that are talking about it, but not necessarily enough people feeling comfortable about that conversation.
And it's something I've spoken about very openly since mom died just because, you know, you have to follow these things through.
So she had noticed that there had been a change.
She had gone to the doctor.
They sent her for a blood test, but life and parenting and work sort of took cover as ever.
And she didn't go for the blood test when she should have gone for that blood test.
And then when she did finally go, by that point, it was a later diagnosis, which wasn't ideal obviously.
And I think that we've just got to get to know our bodies better.
We just have to, and we have to understand that responsibility lies with us.
No one else knows our body like we know our bodies.
And I still think there's that disconnect with some people to understand that it is about us.
The next step isn't about us.
But that initial step can only ever be about us.
You can have a long lasting relationship with somebody who could perhaps notice something different in you and how you look, for instance, your energy levels for example.
But knowing your body, knowing the lumps and bumps and changes within your body and your bodily functions, only you can know that.
And we have to get to know our bodies better and feel comfortable with knowing our bodies better.
And I still think there's that disconnect that we just have to get over.
Yeah, we need to be actively looking for change rather than a change be so significant that we can't ignore it anymore.
Or you know, it gets to the point where somebody else is spotting that you're losing weight or then, you know, you really, I think if people are honest, they knew that something wasn't right before that point.
And cancers are different.
Bowel cancer is one of the types of cancer that not always, but often will give you a clue.
So with the symptoms, change in bowel habit, blood in the stool, you know, feeling tired, feeling weak.
So like breast cancer, you know, breast cancer, if we are regularly checking our breasts, we stand a reasonable chance of picking something up early.
Whereas there are other types of cancer that are deep inside the body like pancreatic cancer, ovarian cancer where actually, it is really difficult and often they're not picked up until they're very late.
So with something like bowel cancer, if it gives us a clue, if it gives you a clue, please act on that clue.
You know, please do something and be looking for it.
Be a detective with your own body.
Now, your mum was very, very young and I know you're approaching the age now that she was when she was diagnosed.
And you have a three-year-old daughter, like she had a three-year-old son.
How does that feel for you?
It feels weird.
You know, one of my best friends is currently having treatment for cancer at the moment.
We're the same age and our kids are of a very similar age.
And I see him and it absolutely breaks my heart because I have more of an understanding now than I did before of how that feels when you think you won't get to see your kids, I don't know, walk down the aisle, have children, you won't see them as adults.
You know, my mom never saw my brother and sister as an adult.
I'm the only one that she saw was able to see through to finishing studying, getting her first job.
I'm the only one that she got to see happen.
She had no idea what my sister was got to become, who my brother was got to become.
She never saw any of that stuff.
And I understand now how hard that is.
You know, you put the work into these little people and you don't get to see it through and you know how heartbreaking it's going to be for them.
And you just have to hope that you've given them enough tools to be able to cope with life and the knowledge that if you haven't, there's absolutely nothing you can do.
And as I approach that age of her being diagnosed, I understand better how utterly devastating that must have been for her.
Yeah.
Yeah.
Are you, because there's a family history, do you have surveillance?
Do you have any tests?
Yeah, I have been tested before because I was very worried about my bowel movements.
This was pre-kids.
I was very worried about my bowel movements and I did go and get tested.
I had the probe up and everything because you know, you have to be armed with knowledge.
As I said, you see something change, you go and get it sorted out.
In my situation, there wasn't anything wrong.
I was very fearful of testing in my 20s.
So I very naughtily kept putting off having my smear test because at that point, I just sort of thought, I'm not ready to have anything else go wrong.
And I just thought if I pretend that nothing can ever go wrong, then I'll be fine for a few years 'cause I just wasn't ready to have to deal with any health issues with myself in my 20s.
I just wasn't.
I was tired of visiting hospitals.
I was tired of lying in hospital beds while someone was having treatment.
I was tired of my family having to deal with loss, of having to deal with illness.
I was tired of everybody having to rear end their lives because someone was ill.
So I just thought if I just put off having my smear test, then if anything is wrong, then I'll deal with that later on down the line.
How do you feel about that now?
Oh, I regularly go for smear tests now.
So then I started having my smear tests in my late 20s, which obviously, I should have been doing it earlier than that because I just had to have a conversation with myself and just say, this is stupid because if something is wrong and I've been putting it off, when something happens, it really is my own fault.
And then I'm leaving my brother and sister without someone again.
So I had to have a conversation with myself and talk myself off a cliff and just say I need to start getting my regular tests done and I'm fine with it now.
I just had a moment where I just like, I just can't deal with anything else going wrong.
So I decided to stick my head in the sand.
I think that's common though.
That is really common.
One of the number one reasons why people don't attend screening and I guess cervical screening is the one that I am most familiar with because we start screening women when they're young.
One of the commonest reasons is if something's wrong, it's the fear of finding out.
This complex, the fear of finding out.
What would you say now you're through that and obviously, the reasons, you had the fear of finding out were way bigger than most people.
But what would you say to somebody listening to this podcast who is putting off going for their smear test or who has got some symptoms but they're putting off because they're so afraid of finding out something bad?
I'd actually say two things.
The first would be you've got to get over yourself.
And the second would be it's not just about you because cancer isn't just about the person that's going through the treatment who is hit physically with that.
It's not just about the individual, it's also everybody else that's around them because the diagnosis and the repercussions of that never just affects one person.
It affects a whole load of people, some who are blood related, some who aren't.
So it's the understanding it's not just about you.
Everybody around you is impacted by that diagnosis and all those people around you would rather have you around than have to bury you.
I think that's really good advice.
I'm got to pass that one on to my dad because bowel cancer affects my family too.
So my dad lost both his mum and his sister in their early 60s.
And is he getting tested?
And my dad will not get tested.
And that's very much a conscious decision?
And his daughter is a GP and we've had lots of conversations about it.
But I think it's that it's a combination of what I call the Superman complex, which I think probably is quite common amongst men.
That he feels he's fine, he's healthy, you know, he feels very confident there's nothing wrong, so therefore, no need to be tested, combined with actually the fear of if there is something wrong, finding out.
And I think the advice I often give to people around that is well, if there is something wrong, you're got to find out at some point.
So you might as well as have that fear and worry about it then and not worry about it now, just get the test done.
Chances are it'll be normal and you'll be fine and then you can stop worrying about it all together.
But the importance of finding out early versus finding out late can be the difference between life and death, but also the difference between the types of treatments that you need to have.
And very early, as you mentioned right at the start, if bowel cancer is found very, very early, it can actually be treated with a very small operation and has very, very good outcomes.
But then how's it feel for you that you're not able to push him to do that?
'Cause you know better than anyone what the ramifications of that is.
It's frustrating and I know with my dad that, you know, at the end of the day, it's his decision, as it always is with healthcare.
And I bring it up and we chat about it every now and again.
And his older brother has done the same and chatted about it every now and again.
But it's almost like I don't want to push too far because that could put him off even more.
But I think, you know, having had this conversation with you, Charlene, I'm definitely got to make him listen to this podcast.
Tell him Charlene says he's got to do it.
Tell him, Linton, say.
Linton, go and get yourself tested.
Thank you.
(both chuckling) Thank you so much.
I think on this, I think that's perfect time to bring in our Bupa experts and you know, chat a little bit more about the signs and symptoms of bowel cancer and make sure that our audience are armed with the knowledge of what to do.
Okay, welcome back, everybody.
We're joined now by Petra Simic, who's medical director at Bupa Health Clinics, who's got to share her expertise with us from a medical standpoint.
First of all, Petra, could you let us know a little bit about your experience within the field of of bowel cancer?
Sure, Zoe.
So it's great to be here to talk to you and I think it's been really powerful talking about this.
I'm a GP and have spent the best part of 20 years looking after patients.
So my experience is more in people coming to see me as a GP and either coming with problems related to their bowels or more commonly failing to mention the problems they have with their bowels.
So it's true that doctors love talking about poo and I used to do a lot of children's medicine so I call it poo within my consultations, you know, not stools 'cause that's not a word that people use to describe bowel movement.
So yeah, we talk about poo all the time as doctors, but it's amazing how many people feel really uncomfortable doing that.
So my experience is exactly in the space that we want people to come to when they've got concerns to talk about bowel movements.
Let's talk about it.
Now, you've listened to the conversation that Charlene and I have just had.
Was there anything in that conversation that you sort of wanted to comment on or add to or correct or you know, add some more medical depth to that you think people would benefit from?
So I thought there were a number of things that really stuck out to me.
I think the first thing to say is your mum's experience and your experience is unusual.
So getting a bowel cancer diagnosis under 50 is unusual.
And I think that's important to state because some of the big advocates of this recently, such as Dame Deborah was young.
And so interestingly, what I've seen is more young people worried about their bowels, which is, in theory, a good thing because of early awareness, but less old people thinking that it's something that is relevant to them.
And yet we know the majority of bowel cancer affects people over 50 and actually, over 85 is the most common age group.
And I think that for me is a really important message.
Any cancer diagnosis is traumatic and distressing.
But definitely within my practise, I often find that older people just put these things down to ageing.
So come and go, "Oh yes, well, my bowels aren't right but you know, I'm getting on a bit.
" Or they keep that very private.
So one of the things I'd like us to make sure that we consider is that the older you are, the more likely you are to get any cancer generally, but particularly, bowel cancer.
So I think that's probably something important to discuss.
Yeah and I guess to add to that, IBS, irritable bowel syndrome, is a very, very common condition.
But in people over the age of 50, it's quite unusual to get IBS for the first time over the age of 50, 'cause I know I've had patients in the past come to see me and they're like, "Well, everyone's got IBS?
I just thought it was a bit of IBS.
I've been stressed and I know that that can be linked.
" But if you're over 50 and getting symptoms that you think you would quite like to pass off as IBS, it's less likely to be IBS if that's your age group.
100%, so young people, IBS is top of the list of a condition that may give you bowel disturbance.
Over 50, very uncommon.
And often I see people over 50 who said, "Oh, I've just had an upset bowel, I've had an upset tummy" but they'll talk about it having gone on months.
So another really important thing 'cause we talk about changes in bowel habits being a really important sign of bowel cancer and a change in bowel habit is a difference from normal for you, which is persistent.
You can have very variable bowel habits depending on what you've eaten or drunk or even your level of exercise.
It can massively vary.
Or your menstrual cycle as well for women.
Absolutely.
It can vary a lot with your menstrual cycle.
Completely, women get diarrhoea commonly associated when they start their period.
But what we're thinking about is changes that are persistent over more than a few days and certainly anything over four to six weeks, you really need to talk to your doctor about.
But yeah, you're right, there are other things that can cause disruptive bowels as well.
And I think that really ties into what Charlene was saying earlier.
For each of us as individuals, it is our responsibility to know our normal so we can spot when something has changed.
But if you do have a persistent change that has stuck around for weeks, and especially if you get that inkling, which we often do, that gut feeling that something's not right, well, then it stops being just your responsibility.
It's your responsibility to let the doctor know.
And then you get to share that responsibility with somebody else.
And if you're worried, you know, if you feel like you've ever been dismissed or you've ever been fobbed off by a doctor, don't let it end there.
Ask to see somebody else or see them again and let them know.
You know, if you're really worried, if you've got the inkling you're like, it's our job actually as GPs to try and elicit what your concerns are and what your views are as to what it might be.
So you absolutely have permission and you are allowed to say, "This is what I think it might be, or this is what I'm worried about it being, you know, this is the thing I'd like to be ruled out.
" And that's actually really helpful for us as doctors when you let us know that, isn't it?
Oh, completely, and I do think sometimes, people come into a consultation, they're worried about cancer of whatever type and they don't mention it because A, it's a bit of a test, but also, if they mention it, there's something in their head, if they mention it, it might be more likely to happen.
It's that fear of finding out thing again, isn't it?
So getting them to say, so what were you concerned about is really important because I see people of all ages worried about cancer, and often it's the people least likely to get cancer that are worried about cancer, interestingly.
But having that conversation is really, really helpful.
And then you can go through it.
I think the other thing currently, it used to be that you would have a family doctor that you would probably see fairly regularly.
I think now the way in which we consume healthcare means you might come across a number of different healthcare professionals if you're unwell for a number of weeks or months.
What we're saying is it's really hard to see the same GP twice.
(both chuckling) I mean, yeah, that's very concisely put.
Me dancing around it.
That's the truth.
Yeah.
And as a result of that, you might be the only person in the room that knows this is your seventh, eighth, 10th week of symptoms.
So say it, get it out there, tell someone how long it's been going on for.
If people have already done tests, tell them, 'cause you might have even had tests in a different environment, but let the healthcare professional know exactly how long it's been going on for.
And probably even more importantly, if you have a family history.
So getting to know, not just yourself but your family.
And if someone did die of cancer, sometimes people don't even know what cancer it is, even if it's a close family relative.
I'm always surprised when they say, "Oh yeah, my granddad died of cancer.
" You go, "What type?
" "Well, I don't know.
" Yeah, I'd be interested to ask you about that, Charlene, actually.
Within your family and you know, this army of people, was it known that it was bowel cancer?
'Cause I know when my grandma died of bowel cancer, it wasn't really discussed or talked about.
I think she was quite open about it.
Yeah.
She was quite open about it.
I mean, I always say that we were quite a cancer family, that my nanny had lung cancer.
She died from lung cancer and my uncle had it in his foot on his heel.
He developed it.
So it's something that travels through, but my mom was very open about it.
But types of cancer, really important.
But you're right, some things are a real taboo.
So often gynaecological cancers and bowel cancers, for men, kind of testicular or penile cancers, all of these things are like not just cancer, which is a taboo on its own, but God, an embarrassing part of the body cancer, even worse.
And it's important if we know there's a strong family history, and by that, I mean probably more than one person that's close to you or anyone young that we dig in a little bit more to that.
Around five to 10% of bowel cancers have a genetic component.
So it's not a lot, but anyone that thinks, oh, there seems to be a cluster, more than one or someone particularly young, have a chat with your GP.
You may be eligible for earlier screening or more intense screening in the general population.
Well, Charlene, your children are very young at the moment, but have you thought about when they're older, how you'll talk to them about the fact that there's cancer in the family and?
It'd be something that that I'd be very open about.
I have no issue talking about cancer at all.
Hence I do stuff like this because I think it's very important that people realise it's something you can be comfortable discussing 'cause discussing it is what saves lives.
So I will have no issue about doing that whatsoever.
And I'm a big supporter and believer in talking very openly to people around me generally in life.
And you know, like I'll push my partner if anything's different with him, I'll push him to go and get tested and what have you.
I'm very, very open about it.
And I feel like generationally, a younger generation, as you say, is a bit more open about talking about various different types of cancer because we are having conversations about it in a way that my parents' generation never did.
My grandparents' generation never did.
It was stuff you were supposed to be embarrassed about for some reason or another.
And I feel like as we go on generation after generation, people generally are more open about talking about lots of different things regarding their bodies.
Yeah, and I think as we dampen down that stigma, we save lives.
And I think, also now, we have access to information.
You know, when we were young or when when your parents, when you were young and your parents were looking after you, they couldn't just google it.
Did you have one of those big encyclopaedias that A to Z of all the medical conditions?
Yeah, no, we had like the big A to Z encyclopaedia that went all across our shelves, which, you know, they died a death, didn't they?
'Cause of Google.
But yes, we didn't have that.
You couldn't google bowel cancer to get more information about it at that point in 1996.
You just couldn't.
So, you know, all we had were our GPs to have a conversation with about it.
They were our source and fountain of knowledge.
That's when you could see a GP, right?
We had a brilliant, do you know what?
We had a brilliant, brilliant, brilliant GP back in the days where you could see the same GP all the time.
And our GP surgery was amazing.
We've got our GPs by the way.
We just need more.
There just needs to be more others and then we'd be fine.
Yeah, okay, well was there anything else, Petra, that you picked up earlier?
Do you know, I think the other thing that really struck me in the conversation was the most amazing conversation about death.
Yes.
And it's something that was really enlightening and uplifting.
Yeah, it was.
And I think we need to get better at talking about what does a good death look like?
Because we will all experience death.
It's the one thing that's guaranteed.
The only one thing is absolutely guaranteed we will experience.
And what I took away from that was just how much we can control the environment surrounding death.
So the conversation around it, knowing what people want when they're going through that process and not being scared of it.
And I think that was wonderful to hear your experience, really, really joyous and I'm sure exactly and entirely as your mum intended, which is I think without a doubt the most important thing.
But I think that for me was really fascinating.
When we think about how we deal with death now, I still think that's a massive taboo.
Yes, oh it absolutely is.
Yeah.
Yeah.
Most, definitely.
And the people do find it strange in Jamaican culture that we do see it as a celebration, that my mom's funeral, we had a DJ, we had a caterer, you know, people partied until the church hall closed at, I don't know, half past 10.
Everyone decamped back to our house.
I think it was still going at like 2, 3 o'clock in the morning 'cause it is an absolute celebration.
But then when you talk to people that aren't used to that, they do find that quite strange.
But that's my normal because you know, when someone's gone, it's sad.
But you also have to celebrate what a brilliant life they had when they were here.
100%.
I have no doubt that when my mum listens to this, she'll be saying that's what I want.
Yeah, yeah, yeah.
(all chuckling) She's always said, by the way, if anything, like,, I want a really massive party.
She'll be saying, you know, that description?
That was exactly it, Petra, that is precisely it.
I'll hand you some good detail then.
Yeah, so I've been taking some notes, not that there's anything wrong with them, they're in great health, but yeah.
But it was interesting how you sort of preempted that part of the chat by saying now people might find this strange, but, but I think most people actually, especially the way you put it and you really painted that picture, I think a lot of people hopefully will take away from this conversation that the positiveness from that and the joy from that.
And you know, we all fear death.
It is the only inevitable thing.
But actually, yeah, painting that picture of all the things that can be good around it, you know, that absolute warm soft blanket that you had in the people that were around you made what was the most devastating thing of your life a joyous memory.
I think that's really powerful.
Yeah, as you sort of said, Petra, we don't really like talking about death, but I think the more openly we talk about it, the more joy we can get from it because you know, either way, it's gonna be awful but if you can sort of take even just a tiny bit of joy from that, I think it helped you later on down the line in terms of the way that you processed it.
Well, it's been a joy having both of you on the podcast.
Thank you so much, Charlene for sharing all of that, honestly.
Thank you so much.
And then Petra, also for what you've added.
Thank you.
My hope is that there'll be loads of people out there, firstly have loads of people listening to the podcast and secondly, loads of people, you know, reevaluating some of their decisions, some of their fears, whether that's around screening, whether it's getting that thing checked out that's been niggling.
And hopefully, you know, we might have just saved some lives.
Hopefully.
Thank you so much.
Oh, thank you.
(guests clapping) Yay.
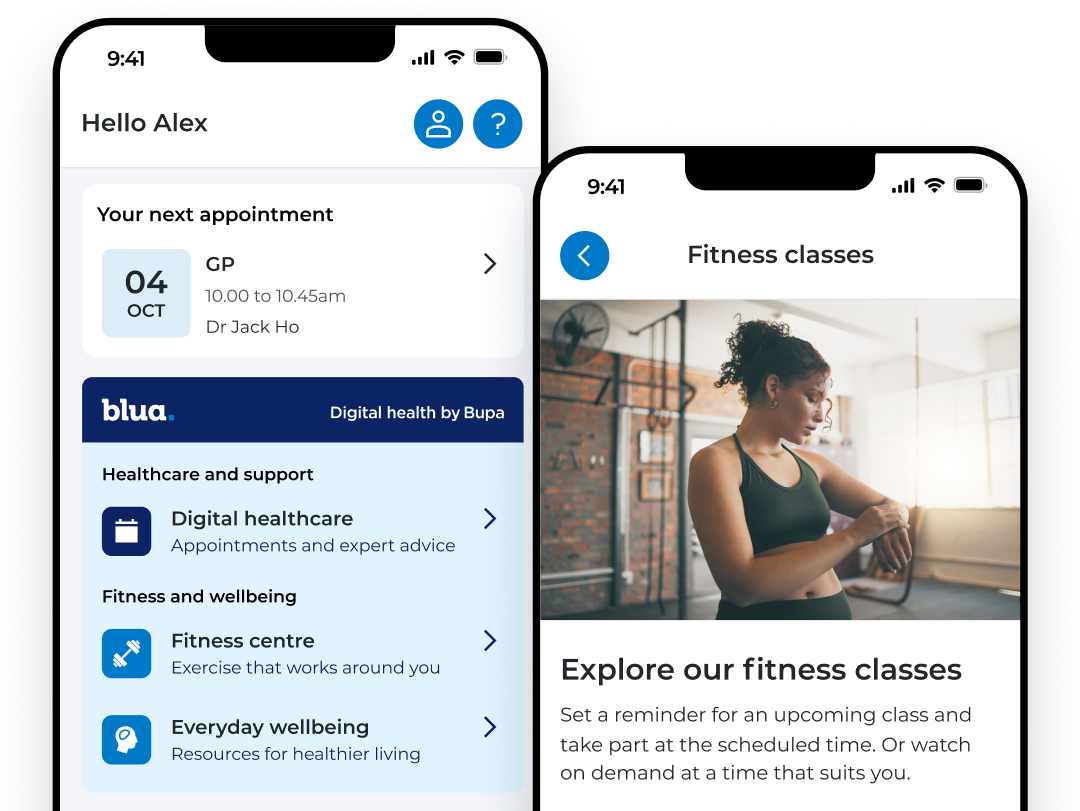
My Bupa, everything your people need in one place.
A digital account provides a convenient way for your people to get the support they need. Personalised to your employees level of cover, they can access a range of resources and services available to them.
To sign into the My Bupa app, your employees can use their existing Bupa account, or by creating a new digital account.
Scan the QR code with your phone camera to download the app.
Further resources

Understanding cancer
Understand different cancers and get support if you or someone close has a diagnosis. Plus, find information on common symptoms and treatment.

Healthy Me. Blog
Designed to help you live a healthy lifestyle, find help and advice from our experts on a range of topics.





