Epidural injections for lower back and leg pain
Your health expert: Mr George Michael Hess, Consultant Trauma & Orthopaedic spinal surgeon
Content editor review by Pippa Coulter, Freelance Health Editor, October 2023
Next review due October 2026
Epidural steroid injections can help relieve pain in your back or legs caused by sciatica. It involves a minor procedure in hospital to have an injection in your back.
About epidural injections
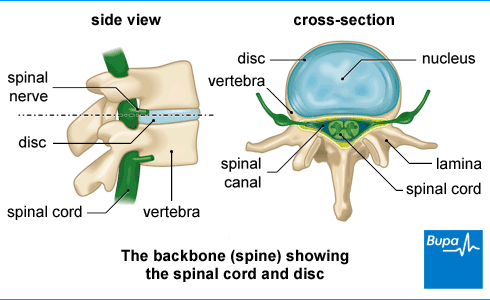
An epidural injection contains a steroid medicine, usually together with a local anaesthetic. These injections are also called epidural steroid injections. The liquid is injected into a gap called the epidural space, which surrounds your spinal cord. The steroid works by reducing inflammation around your spinal cord. The local anaesthetic provides faster pain relief.
Epidural injections may not completely cure your pain. But they may help to relieve your pain in the short term. This can last for up to several months at a time. Even if you only have pain relief for a short time, this can help you to get on with your normal daily activities and keep active. Being active is important for improving your pain in the long term or preventing it coming back. If the injection helps to reduce your pain, it may also reduce the need for more invasive procedures, including surgery.
A nerve root block is a similar type of procedure to an epidural injection. This involves having an injection at a nerve root, where a nerve exits the spine. It’s used to confirm whether there is a problem with one particular nerve. It may also provide some pain relief.
Uses of epidural injections
Epidural injections can help with sciatica (radicular pain). This is pain that spreads from your lower back down your legs. It’s caused by a trapped nerve in your spine. There are several things that can cause this including the following.
- A slipped disc (herniated disc). This is when one of the discs between your vertebrae (back bones) bulges out of your spine, sometimes pressing on surrounding nerves.
- Spinal stenosis. This is when the space around your spinal cord narrows, putting pressure on your spinal cord.
- Spondylolisthesis. This is when one of your vertebrae moves out of position.
Your GP will usually suggest other things you can do to manage sciatica pain before recommending epidural injections. These include keeping active, using heat, taking painkillers, exercise programmes and physiotherapy. If your sciatica is severe and doesn’t improve with other treatments, they may refer you to a spine or pain specialist. They can assess you and advise whether epidural injections might be a good treatment option for you. You may also be able to book an appointment directly with a private consultant trained in epidural injections. You’ll need to pay for this.
Epidural injections aren't a suitable treatment for everybody. If you’re on blood-thinning medication, have an infection, have diabetes or could be pregnant, let your doctor know. They may need to make extra preparations or postpone your injection. Also, tell your doctor if you’ve had an allergic reaction to previous injections or if you have a bleeding disorder.
If your doctor offers you an epidural injection, they’ll discuss with you exactly what to expect. This will include all the potential benefits and risks. Be sure to ask your doctor if you have any questions or need any more explanation. You'll need to give your consent if you do choose to have the injection, so it’s important that you feel fully informed.
Preparation for an epidural injection
Your doctor will explain how to prepare for your procedure. A pain specialist or spinal surgeon will carry out the injection. You have the procedure as a day case in hospital. This means you have the injection and go home later the same day.
You may be offered a sedative for the procedure. This will help you to relax, but you’ll stay awake. You won’t be able to drive straightaway after the injection. Make sure that you arrange for someone to drive you home, and preferably stay with you overnight.
You may be asked to stop eating and drinking for several hours before having an epidural injection. You’ll usually still be allowed to have clear fluids up to a couple of hours beforehand. Follow any instructions given to you by your doctor.
Tell your doctor about any medications you’re on. If you’re taking any medicines, particularly blood-thinning medicines, you may be asked to stop taking these for a few days before the procedure. Never stop any medication unless your doctor tells you to.
Having an epidural injection
At the hospital, your doctor will explain what will happen and check that you’re still happy to go ahead. They’ll ask you to change into a hospital gown. When they’re ready to start, your doctor will ask you to lie on your front, on a special table.
Your doctor will place a cannula (fine tube) in the back of your hand. This is to give you a sedative, if you are having one, and in case you need any other medication during the procedure. Your doctor will then carefully clean and prepare the area on your back where you're having the injection, using an antiseptic solution. Your doctor will inject a local anaesthetic to numb the area. This may sting a little.
There are different techniques for giving epidural injections for back and leg pain. These include:
- interlaminar – this is given between two of your vertebrae (back bones)
- transforaminal – this is an injection in an area where a nerve exits the spine
- caudal – this is given through an opening at the base of your spine
Your doctor will guide the epidural needle to the right area in your back using real-time X-ray images (fluoroscopy). To do this, they’ll inject a type of dye, called contrast, to check when the needle is in the right position. Once the needle is in position, your doctor will slowly inject the medication into the epidural space surrounding your spinal cord. You might feel some pressure when you have the injection, but it shouldn’t be painful. Let your doctor know if you do feel any discomfort.
It will only take a few minutes to give you the epidural injection, but the procedure as a whole may take up to 30 minutes.
How an epidural is given
What is an epidural? | the procedure - watch in 1 minute 37 seconds
An epidural is an injection into your lower back to temporarily block pain from your waist down. This video describes how an epidural is given.
An epidural is an injection into your lower back that temporarily blocks pain from your waist down.
You'll be asked either to lie on your side with your knees tucked into your chest, or to sit upright and lean forward.
This opens up the space between the bones in your spine.
Your anaesthetist will carry out your epidural in two parts.
Firstly, a small amount of local anaesthetic is injected into your skin to completely numb the area.
Then, a hollow epidural needle is given into your epidural space.
This is the space just outside the membranes that surround your spinal cord.
When the epidural needle reaches the correct spot, your anaesthetist will thread a very thin plastic tube through the centre of the hollow needle.
They'll then remove the epidural needle, leaving just the tube in place.
The tube will run from inside your epidural space to the outside of your body.
It's secured using adhesive tape and used by your anaesthetist to give you medicines for pain relief when you need them.
Your anaesthetist may also attach a pump to the tube so you can top up your pain relief when needed, and sometimes you'll be able to control this yourself.
When you no longer need pain relief, the tube will be carefully removed and the area covered with a plaster.
Aftercare following epidural injection
Your doctor or nurse will take you to a recovery room or area after the procedure. The nursing staff will monitor you for a short time before you're able to leave. Sometimes, they’ll ask you to lie flat for around 30 minutes or so. They may check your blood pressure or pulse, and ask if you're experiencing any side-effects. The nursing staff will make sure that you can stand up safely when you feel ready.
You'll usually be able to go home within a few hours after your injection, and sometimes much sooner. But you’ll need somebody to drive you home – you won't be able to drive yourself. Ideally, you should also have someone stay with you for the first night after your procedure, especially if you have had a sedative.
It can take several days to feel any benefit from the injection. In fact, some people find that their pain gets worse at first. This should settle down within a few days. Keep taking your usual pain medications. Try to keep as active as you can, and as your pain improves, you can gradually increase how much you do.
Pain relief from epidural injections
Epidural injections help many people who have pain due to sciatica. But it’s important to realise that it doesn’t work for everyone, or the effects may only be very small. How well it works depends on many factors. These include what has caused your sciatica and how long you’ve had symptoms. The injection is more likely to work if you haven't had symptoms for very long. The success rate of epidural injections also varies between doctors and depends on the technique they use. Ask your doctor how these factors apply to you.
If you do get pain relief from an epidural injection, it tends to be short lived – only lasting for a few weeks or months at the most. For some people, this may be long enough to recover from the cause of their pain. The amount of pain relief you get and how long it lasts varies from person to person. If you’ve found it helpful, your doctor may recommend you have repeat injections (usually up to three or four per year) until the pain has gone. You’ll need to wait at least two weeks between injections.
Side-effects of epidural injections
Side-effects are unwanted but mostly temporary effects that you may get after a procedure. The main side-effect associated with epidural injections is mild discomfort in the area where you have the injection. This usually gets better on its own within a few days.
Some people have a reaction to the medicines used in the injection. For instance, your face may look flushed or feel warm. Some people feel sick or dizzy, and may faint.
It's possible for the local anaesthetic from the injection to spread, causing temporary numbness or weakness in your legs. This should get better very quickly.
Complications of epidural injections
Complications are unexpected problems that can happen during or after the treatment.
More serious complications from epidural injections are rare, but it's important to be aware of them. They include the following.
- Infection, which can spread to your spine. This is rare, but you’re at greater risk if you have diabetes or a weakened immune system. If the injection site becomes warm or red and you feel hot and unwell, contact the unit where you had the injection. They can give you antibiotic treatment.
- A dural puncture. This is when the needle has gone too far and entered the spinal fluid. You may develop a severe headache as a result. If you develop a headache after you've got home, take some paracetamol and lie flat. Contact the unit if it carries on for longer than 24 hours.
- Bleeding into the epidural space (a haematoma). This is rare (affects between 1 and 2 in 10,000 people), but it can be serious. If it did happen, you would need surgery to deal with it.
- Injury to a nerve. This can cause ongoing weakness in your legs and incontinence. This will need urgent investigation in hospital. Serious injury is very rare.
Your doctor will have measures in place aimed at keeping the risk of these complications as low as possible.
Alternatives to epidural spinal injections
Most episodes of sciatica get better on their own in time, without the need for injections or other invasive treatments. There are many other methods for managing the pain, including painkillers and physiotherapy. You might decide to try or continue using these options rather than have an epidural injection. Your doctor will go through your treatment options and help you to decide what’s best for you.
Physiotherapy services
Our evidence-based physiotherapy services are designed to address a wide range of musculoskeletal conditions, promote recovery, and enhance overall quality of life. Our physiotherapists are specialised in treating orthopaedic, rheumatological, musculoskeletal conditions and sports-related injury by using tools including education and advice, pain management strategies, exercise therapy and manual therapy techniques.
To book or to make an enquiry, call us on 0345 850 8399
Epidural steroid injections give short-term pain relief. If it works for you, it may last for up to several months. This is different for everyone. Some people only get a small amount of pain relief or it doesn’t last for very long. For some people, it might not work at all. Find out more in our section on pain relief from epidural injections.
There are some side-effects from having epidural injections, like soreness or mild discomfort where you have the injection. It may also cause temporary numbness or weakness in your legs. More serious complications include things like an infection and injury to a nerve, but these are rare. You can read more about the potential risks in our sections side-effects of epidural injections and complications of epidural injections.
You'll have a local anaesthetic to numb the area, so it shouldn’t be painful when you have the injection. You may just feel some pressure as the doctor injects the medication. It can be a bit sore at first afterwards, but this will pass within a few days. Read more about what to expect in the section having an epidural injection.
It can take a few days before you feel any benefit from an epidural injection. Some people find that the pain gets worse before getting better. You can take the usual painkillers during this time. Find out more in our aftercare section.
Local anaesthesia
Local anaesthesia involves numbing a small part of your body with a medicine called a local anaesthetic to stop pain during and after surgery.
Corticosteroids
Lower back pain
Lower back pain is very common. It is often caused by straining muscles, tendons or ligaments in your back. Find out everything you need to know about lower back pain.
Physiotherapy for lower back pain
Did our Epidural injections for lower back and leg pain information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Low back pain and sciatica in over 16s: assessment and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 11 December 2020
- Epidural steroid injection for the treatment of pain. Faculty of Pain Medicine, Royal College of Anaesthetists. www.fpm.ac.uk, reviewed September 2022
- Hassan KZ, Sherman AI. Epidural steroids. StatPearls. www.ncbi.nlm.nih.gov/books /, 19 July 2022
- Epidural steroid injections. Medscape. emedicine.medscape.com, updated 9 May 2022
- Chang D, Zlomislic V. Chapter 273. Lumbar Spinal Injections. In: Chapman MW. Chapman's Comprehensive Orthopaedic Surgery. 4th ed. 2019. New Delhi: Jaypee Brothers Medical Pub
- Sciatica (lumbar radiculopathy). NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2022
- Transforaminal epidural/ nerve root block/dorsal root ganglion block for the treatment of pain. Royal College of Anaesthetists. www.fpm.ac.uk, updated September 2022
- Personal communication. Mr George Michael Hess, Consultant Trauma & Orthopaedic spinal surgeon, 9 October 2023
- Recommendations for good practice in the use of epidural injection for the management of pain of spinal origin in adults. 2nd ed. Faculty of Pain Medicine, Royal College of Anaesthetists. www.fpm.ac.uk, published March 2021
- Sedation for procedures for the treatment of pain. Royal College of Anaesthetists. www.fpm.ac.uk, updated September 2022
- Oliveira CB, Maher CG, Ferreira ML, et al. Epidural corticosteroid injections for lumbosacral radicular pain. Cochrane Database Syst Rev 2020;4(4):CD013577. doi: 10.1002/14651858.CD013577



