Lower back pain
- Dr Sundeept Bhalara, Consultant Rheumatologist
Lower back pain is pain and stiffness in the area of your back from the bottom of your ribs to the top of your legs. The cause isn’t normally serious and you can often manage lower back pain yourself. But for some people, it’s important to get advice from a physiotherapist or doctor.
About lower back pain
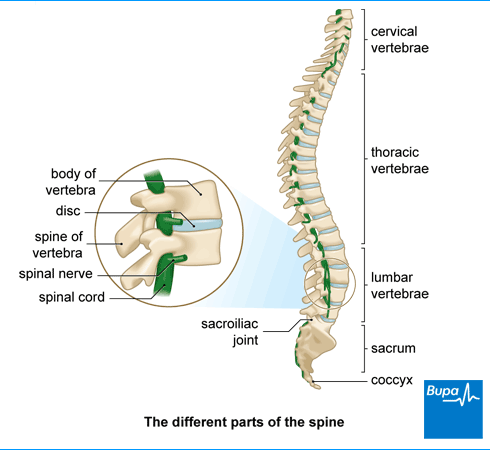
Lower back pain can come from any of the many structures that make up your back. These include bones, joints, muscles, ligaments, nerves, and tendons.
Your spine supports your back. It’s made up of 33 segments of bone called vertebrae that are stacked on top of one another. The lower section of your spine is called the lumbar spine. Below the vertebrae, at the bottom of your spine, are bones called the sacrum and coccyx. You may hear lower back pain referred to as lumbosacral pain.
Discs of cartilage sit between each vertebra, which act as shock absorbers and allow your spine to bend. Lower back pain can originate from these discs. Your spinal cord threads through the vertebrae, and carries nerve signals between your brain and the rest of your body. If nerves at the base of your spine become compressed (a pinched nerve in your lower back) or inflamed, it can cause sciatica. Sciatica is a type of pain that starts in your back or bottom (buttocks) and spreads down your leg.
It’s difficult for doctors to find the cause of back pain because there are so many different parts to your back and tissues that surround it. Even tests, such as X-rays and magnetic resonance imaging (MRI) scans aren’t helpful for most people.
Lower back pain is very common – around 4 in every 5 people have pain in their lower back at some point in their life.
Causes of lower back pain
Lower back pain can be classed in two different ways: specific back pain and non-specific back pain.
Specific back pain
This is when you have a specific cause of your back pain, which can include the following.
- A slipped (herniated) disc. This means one of the discs between your vertebrae bulges out of shape and presses on the surrounding spinal nerves. It’s a common cause of sciatica.
- A crack or break (fracture) in one of your vertebrae. This can happen after trauma to your spine (such as an accident), or if you have osteoporosis (a condition that weakens your bones).
- Facet joint pain. This is pain in one of the joints that link the bones in your spine together.
- Inflammatory lower back pain. This can be caused by a condition such as ankylosing spondylitis , which causes inflammation in your spinal joints and ligaments.
Sometimes, you may feel problems that affect other organs in your body, such as your kidneys, pancreas or bowel, as back pain. And occasionally, a more serious condition, such as an infection or cancer, can cause pain in your lower back. These are much less common causes of lower back pain.
Non-specific back pain
This means no particular cause can be found for your back pain. It’s by far the most common type of back pain and is often a strain of the muscles, tendons or ligaments around your back.
While it’s not always possible to say exactly what the cause of your back pain is, certain things can increase your risk. These include if you:
- lifting heavy or awkward objects
- are obese
- are inactive
- having a demanding job, or are stressed due to work
- stand for a long time
- are depressed
- smoke
Symptoms of lower back pain
Lower back pain symptoms can vary from person to person. Lower back pain may come on suddenly, after you lift something heavy or move in a way that hurts your back, for example. Or it may come on gradually over time, or for no clear reason.
Some people get a dull pain in their back, while others describe it as more of a tearing or burning pain. You may find certain things make the pain worse, and other things help to relieve it. The pain can range from mild, to severe lower back pain.
If you have sciatica, pain can spread from your back or buttock down your leg, sometimes as far as your foot or toes.
Seeking help for lower back pain
You might not need to seek help from a health professional to get lower back pain relief. Most people find their lower back pain improves by itself within a few weeks or so. But if there's no improvement after six weeks, or the pain is getting worse, seek advice from a GP, physiotherapist, or osteopath. It's also worth calling them if back pain stops you from doing your normal activities.
Physiotherapists can help with back pain. In some areas, you may be able to self-refer to a physiotherapist on the NHS, whereas in others you need a referral through your GP. You can also choose to pay for private physiotherapy.
Sometimes you should see a doctor straightaway for lower back pain, for example if:
- you’ve been in a major accident, such as a traffic accident or fall
- you have numbness or tingling around your bottom or genitals
- you have sciatica pain in both legs
- you can’t control your bladder or bowels (when you pee or poo), or can’t pee
- you’re unsteady when you walk, or your legs or feet feel weak
- you have sudden, severe lower back pain
- you have osteoporosis
- there’s something that you can see is wrong with your back – you have a visible deformity
- the pain continues when you lie down or overnight, which disturbs your sleep
- you have a history of cancer or have had a recent bacterial infection
- you also have a fever, chills or unexplained weight loss
These can be signs of more serious problems.
Diagnosis of lower back pain
Your physiotherapist or GP will usually diagnose lower back pain from your symptoms and by examining you. They’ll want to rule out any underlying problem that could be causing your pain.
Your physiotherapist or GP will ask you lots of questions about your lower back pain. These may include when it started, how bad it is and if there’s anything that makes it better or worse. They may press against your back to see if there’s any tenderness, and check to see how it looks. They might ask you to move around too, to see if you have any problems when you bend or extend your back.
Further tests won’t usually help. But if your symptoms indicate an underlying problem, your GP may recommend tests, which may include:
They may also refer you to a specialist for further investigations.
Self-help for lower back pain
There are things you can do to get some lower back pain relief, and recover faster. The most important are to keep active and to try to stay positive about managing your pain.
Keeping active
You might feel that you shouldn’t do too much if you’ve got back pain, or that exercise might make it worse. But actually, keeping active will help you to recover faster from back pain. Too much rest can stiffen your joints and weaken your muscles, which can increase your risk of long-term problems. If you keep active, it will keep the muscles around your spine strong and your back mobile. Regular exercise can release chemicals called endorphins, which can make you feel better too. You don’t need to wait until you’re pain-free to get moving.
You might get a bit of pain at first, but that doesn’t mean it’s harmful. If you start gently and can manage to put up with any pain, it should start to get better. It doesn’t really matter what you do, as long as you’re active. Choose an exercise that you enjoy. Good examples include walking, swimming and yoga. If you develop severe back pain (that you can’t cope with) when you exercise, stop and get advice from a doctor. Always see a doctor if you have numbness or weakness in your legs.
Pain relief
If you need pain relief, take over-the-counter non-steroidal anti-inflammatory medicines (NSAIDs) such as ibuprofen. Research shows paracetamol on its own doesn’t help lower back pain but it may help if you take it in combination with ibuprofen.
You may find it helps you to keep active if you take painkillers before you do any exercise. But only take NSAIDs for a short period of time – follow the guidance on the patient information leaflet.
You could apply heat or cold (ice) treatments to your back to help relieve pain. Make sure you protect your skin properly if you do.
Staying positive
Recovery from low back pain is strongly linked to how you feel emotionally, and how you cope with the pain. Emotional factors can increase the risk of your back pain becoming long-term (chronic). These include:
- worrying that physical activity and pain is causing you harm
- feeling depressed, anxious, or stressed
- a lack of social support from family and friends
- feeling unmotivated to try treatments for your pain
If you have lower back pain it can be frustrating, but try to stay positive as it can help you to recover faster. Try to keep up with your normal routines and social activities as much as possible. Get out and spend time with friends or do an activity, as it can really help.
Stress can make back pain worse.If this is a problem for you, think about what you can do to manage your stress. Make sure you get enough sleep, as this can make a difference too.
Physiotherapy services
Our evidence-based physiotherapy services are designed to address a wide range of musculoskeletal conditions, promote recovery, and enhance overall quality of life. Our physiotherapists are specialised in treating orthopaedic, rheumatological, musculoskeletal conditions and sports-related injury by using tools including education and advice, pain management strategies, exercise therapy and manual therapy techniques.
To book or to make an enquiry, call us on 0345 850 8399
Treatment options for lower back pain
If you see a physiotherapist or GP for lower back pain, they’ll probably encourage you to try the self-help measures above first. They can also advise you on some lower back pain exercises you can do to help your back, or may refer you to a group exercise programme. If your pain doesn’t improve, they may be able to recommend other lower back pain treatment options you can try, and can refer you to a specialist if necessary.
Medicines
If over-the-counter NSAIDs don’t help, your GP may offer you different medicines for pain relief, to take alongside self-help measures. These may include a medicine called codeine. You should usually only take this medicine for a very short time, as you may become dependent on it. Your GP may also offer you a short course of a muscle relaxant.
Sometimes, your doctor may offer you antidepressant medicines for lower back pain.
Always read the patient information that comes with your medicine. If you have any questions about your medicines or how to take them, ask a pharmacist.
Physical therapies
Your GP may refer you for physiotherapy for lower back pain, or you may be able to refer yourself. A physiotherapist can help in lots of ways with lower back pain. They may:
- give you some lower back exercises to improve your movement, muscle strength, posture, and flexibility
- help with pain management by using various therapies, such as ice, heat, and ultrasound
- provide ‘hands on’ (manual) therapy, such as massage or spine manipulation
You may want to try other options, such as chiropractic treatment or osteopathy for back pain. These treatments aren’t usually available on the NHS. Be sure to do your research before you try anything new and find a registered practitioner.
Psychological therapy
It can be difficult to stay positive when you’ve had back pain for a long time. But if you stay positive and keep active, it can help you recover and prevent back pain becoming long term.
If negative feelings are hampering your recovery, you may benefit from some psychological support for lower back pain. Your doctor may suggest cognitive behavioural therapy (CBT) alongside exercise. This can help you to understand and change the way you react to and cope with pain. You may also find relaxation techniques, such as breathing exercises useful.
Injections and other procedures
If you have severe sciatica, your doctor may suggest an epidural injection. Epidural injections contain a local anaesthetic and steroid to relieve pain and reduce inflammation. They’re only recommended for sciatica and not non-specific lower back pain.
If your back pain is chronic (long-term) and other treatments haven’t helped, your doctor may suggest a procedure called radiofrequency denervation. It’s only suitable for certain types of back pain. Your doctor will refer you to a specialist to assess whether it would help you.
Surgery
Back surgery is very rarely suitable for people with lower back pain. Your surgeon will usually only recommend it for certain types of back pain and if no other treatments have helped. As with every procedure, there are risks of back surgery. Your doctor will explain how these apply to you.
Prevention of lower back pain
If you look after your back, it can help to reduce your risk of getting back pain.
- Get plenty of exercise. If you keep active and do regular exercise, it can help to prevent back pain coming back, or reduce your risk of getting it at all.
- Take care when you lift and carry heavy items. Don’t lift or carry more than you can manage, and use the right technique. This means slightly bending your back, knees, and hips when lifting, rather than stooping from your back.
- Keep a good posture. If you work at a desk, make sure your chair, desk and computer screen are set up correctly. Your employer can assess your workstation.
- Move regularly – don’t sit in the same position for long periods of time.
Medicines checklist
Our handy medicines checklist helps you see what to check for before taking a medicine.
Bupa's medicines checklist PDF opens in a new window (0.8MB)
Lower back pain is often caused by a strained muscle, tendon, or ligament in your back. But it’s often not possible to say for sure what’s caused it. Sometimes there’s a specific cause, such as a slipped disc, fracture, or inflammation.
See our causes of lower back pain section for more information.
Recovering from lower back pain is strongly linked to how you feel emotionally, and how you cope with the pain. If you worry and feel stressed about it, this can increase the risk of your back pain becoming long-term (chronic). Lower back pain can be frustrating, but try to stay positive as it can help you to recover faster. Try to keep to your normal routines and get out and spend time with friends or do an activity, as it can really help.
See our self-help for lower back pain section for more information.
Lower back pain usually gets better by itself and aside from keeping active and managing pain, you usually won’t need any further treatment. But sometimes you may need to see a physiotherapist to get some advice on exercises to do. If the pain is severe, you may need to see a doctor, who may prescribe you painkillers. Back surgery is very rarely suitable for people with lower back pain.
See our treatment of lower back pain and symptoms of lower back pain sections for more information.
There are some red flags for lower back pain – this means that you have symptoms that should be checked with a doctor. These include if you have numbness or tingling around your bottom or genitals, or you can’t control your bladder or bowels (when you pee or poo), or can’t pee. And if you’re unsteady when you walk, or your legs or feet feel weak, or you have sudden, severe lower back pain, get medical help too.
See our symptoms of lower back pain section for more information.
Physiotherapy for lower back pain
Chiropractic for lower back pain
Chiropractic is a treatment where a practitioner called a chiropractor uses their hands to help relieve problems with the bones, muscles and joints, such as lower back pain.
Osteopathy
Osteopathy can help you to manage back pain, neck tension, aches and pains.
Did our Lower back pain information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Musculoskeletal lower back pain. BMJ Best Practice. bestpractice.bmj.com, last reviewed 21 July 2024
- Desai C, Reddy V, Agarwal A. Anatomy, back, vertebral column. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 8 August 2023
- The spine: Anatomy and function. National Spine Health Foundation. spinehealth.org, published 5 December 2023
- Miniato MA, Black AC, Varacallo M. Anatomy, back, vertebral column. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 12 October 2023
- Sciatica (lumbar radiculopathy). NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2023
- Low back pain and sciatica in over 16s: Assessment and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 11 December 2020
- El Sayed M, Callahan AL. Mechanical back strain. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 8 August 2023
- Lumbar herniated nucleus pulposus. MSD Manual Professional Version. www.msdmanuals.com, reviewed/revised October 2022
- Casiano VE, Sarwan G, Dydyk AM, et al. Back strain. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 11 December 2023
- Curtis L, Shah N, Padalia D. Facet joint disease. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 9 January 2023
- Lassiter W, Bhutta BS,Allam AE. Inflammatory back strain. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 26 February 2024
- Axial spondyloarthritis (including ankylosing spondylitis). NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2024
- Back pain – low (without radiculopathy). NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2023
- Find a chartered physiotherapist. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 24 January 2023
- Back pain. Versus Arthritis. www.versusarthritis.org, accessed 24 August 2024
- Mechanical low back pain. Medscape. emedicine.medscape.com, updated 8 May 2024
- Chronic pain. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised January 2024
- Good handling technique. Health and Safety Executive. www.hse.gov.uk, accessed 26 August 2024
- Rachael Mayfield-Blake, Freelance Health Editor



