Testicular cancer
Expert reviewer, Mr Aziz Gulamhusein, Consultant Urological Surgeon
Content editor review by Rachael Mayfield-Blake, February 2023
Next review due July 2026
Testicular cancer is cancer that develops in the testicles (part of the reproductive system). It’s one of the most treatable cancers. Most people make a full recovery, particularly if it’s diagnosed early. That’s why it’s important to contact a GP if you feel anything unusual in a testicle.
How cancer develops
Cancer explained | Watch in 1:48 minutes
In this video, we explain how, when cells divide uncontrollably, this leads to cancer.
About testicular cancer
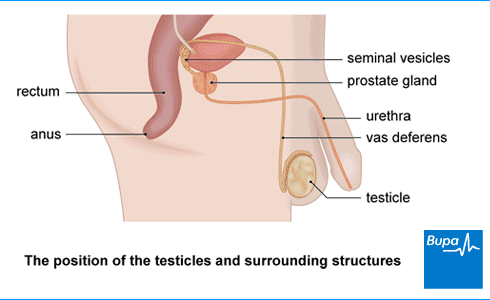
Your testicles lie inside your scrotum, the loose bag of skin that hangs below your penis. Your testicles produce sperm and the hormone testosterone. In testicular cancer, cells in one of your testicles start to grow abnormally and out of control.
Testicular cancer usually affects one testicle. It can sometimes affect both, but this is rare. Testicular cancer can sometimes spread to lymph nodes in your tummy (abdomen) or, more rarely, to other parts of your body.
Testicular cancer is quite uncommon – it affects around 2,400 people in the UK each year. This number seems to be rising and no one is sure why. In the UK, people in their 30s are most likely to get testicular cancer, although you can get it if you’re younger or older than this.
Types of testicular cancer
More than 9 out of 10 cancers in the testicle develop from germ cells – these are the cells that produce sperm. There are two main types of this form of testicular cancer:
- seminoma
- non-seminoma
Seminomas tend to grow and spread more slowly than non-seminomas.
Causes of testicular cancer
No one knows exactly what causes testicular cancer. But there are some things that can make it more likely. The main one is being born with an undescended testicle. This means that one or both of your testicles stayed in your tummy rather than moving down into your scrotum. Your testicles may have moved down later or you may have had an operation to bring them down. If you don’t have this corrected at a young age (some research suggest by 13), you may be even more likely to develop testicular cancer.
Other things that can increase your chances of getting testicular cancer include, having:
- had testicular cancer in your other testicle
- a sibling or parent who has had testicular cancer
- fertility problems and low-quality sperm
White people get testicular cancer more often than those from other ethnic groups, but no one knows why.
Having a vasectomy or an injury to your testicles doesn’t increase your risk of getting testicular cancer. But it may make you notice a lump that was already there.
Symptoms of testicular cancer
Often, the first sign of testicular cancer is a swollen testicle or a hard, solid lump on your testicle. It can be a pea-sized lump on your testicle, or it can be much larger. Usually, you won’t have a painful testicle but you might feel pain or discomfort in your scrotum.
Other testicular cancer symptoms include a:
- pulling sensation or heavy feeling in your scrotum
- testicle that looks bigger than usual
- dull ache or heavy feeling in your lower tummy
- collection of fluid in your scrotum (called a hydrocoele)
Late-stage testicular cancer symptoms include:
- back pain
- coughing or feeling breathless
- weight loss
- enlarged breast tissue
If you have any of these symptoms, contact your GP.
It’s important to regularly check your testicles for any changes and have good testicular cancer awareness. Get to know what’s normal for you so that you’ll notice any changes. The earlier testicular cancer is diagnosed, the better your chances of recovery.
Diagnosis of testicular cancer
If you find a lump or notice something different around your testicles, contact a GP as soon as possible.
Your GP will ask you about your symptoms and examine your testicles. If you have a swelling or lump in your testicle, your GP may refer you to a hospital specialist. This is usually a urologist. A urologist is a doctor who specialises in treating diseases that affect your urinary system and the male reproductive organs.
Your GP may first offer you an ultrasound test. An ultrasound scan uses sound waves to produce an image of the inside of your scrotum and your testicle. It can help to show whether the lump is cancer or not.
Your GP may arrange, or a hospital doctor will offer you the following tests.
- A blood test can check for certain hormones and proteins that can be high if you have testicular cancer.
- The only way to confirm testicular cancer is to have your entire testicle removed. This will be examined by a doctor in a lab to see if there are any cancer cells and if so, what type. Much less commonly, your surgeon may remove only part of the testicle. Ask them for more information about this.
If you’re found to have cancer, you may need to have other tests to see if the cancer has spread, such as a CT scan. This is called staging.
Men’s Health Check
We offer a male health check service to detect the signs of prostate and testicular cancer and advise you should any follow up healthcare be needed.
For further information please call us on 0333 305 7840∧
∧We may record or monitor our calls
Cancer awareness: testicular cancer
Testicular cancer | Watch in 0:34 minutes
This Bupa animation talks about checking your testicles for any lumps or changes and seeing a GP in case this is a sign of testicular cancer.
Treatment of testicular cancer
Treatment for testicular cancer is usually very successful. A team of doctors and other cancer specialists will plan the best care for you. It depends on the type of testicular cancer you have and if it has spread.
Surgery
The main treatment for testicular cancer is surgery to remove your affected testicle (if it hasn’t already been removed during your diagnosis). This operation is called an orchidectomy. If you’re diagnosed early, surgery may be the only treatment that you need. If you just have one testicle removed, you should still be able to get an erection and have children. Your doctor will talk to you about the operation and your options. For more information about your fertility after surgery, see our FAQ: Can I still have children after testicular cancer? below.
You may be able to have an artificial testicle put into your scrotum to give it a normal appearance. Or you could choose to do this at a later time.
After surgery, a team of specialists including an oncologist (a doctor who specialises in cancer care) will look at all your results. They’ll decide if you need further treatment. For example, if your cancer is more advanced, you may need another operation to remove lymph nodes from your tummy. Your doctor will explain everything to you.
Chemotherapy
Chemotherapy uses medicines to destroy cancer cells. It’s usually used to treat testicular cancer if the cancer has spread outside your testicle or has come back after surgery. Even if the cancer hasn’t spread, your doctor may offer you a short course or single treatment of chemotherapy. This is to reduce the chances of testicular cancer coming back in the future.
The type of chemotherapy treatment you have will vary depending on the type and stage of your testicular cancer. Your doctor will give you information on the type and course of chemotherapy that’s best for you.
Radiotherapy
Radiotherapy uses radiation to kill cancer cells. Radiotherapy is mainly used to treat seminoma types of testicular cancer because seminomas are very sensitive to radiation. You may have radiotherapy after surgery to prevent the cancer coming back or to treat any cancer cells that have spread out of your testicle.
Radiotherapy can affect your fertility, so your doctor will talk to you about this before you have radiotherapy. For more information, see our FAQ below: Can I still have children after testicular cancer?
After your treatment
You’ll need to attend hospital appointments and have regular check-ups after your treatment to see if any of the cancer remains or returns. How often these check-ups happen will depend on the type of cancer you had and how it was treated.
Your doctor may monitor your testosterone level and offer you testosterone replacement therapy if your level is too low.
It’s important that you go along for these check-ups because if testicular cancer comes back after treatment, it can often still be cured.
Help and support
Being diagnosed with cancer can be distressing for you and your family. An important part of cancer treatment is support to deal with the emotional aspects as well as the physical symptoms. Your specialist cancer doctors and nurses are experts in providing the support you need. Talk to them if you’re finding your feelings hard to cope with.
You may find it helpful to contact a cancer organisation for further information, support and advice. There may also be local groups where you can meet other people with similar medical issues. Your cancer team may know of some. For contact details of relevant organisations, see our section: Other helpful websites below. You may also find our general cancer articles helpful.
Yes, testicular cancer is very curable if it’s diagnosed early. That’s why it’s important to regularly check your testicles for any changes. Get to know what’s normal for you so that you’ll notice any changes. The earlier testicular cancer is diagnosed, the better your chances of recovery.
The first sign of testicular cancer is a swollen testicle or a hard, solid lump on your testicle. You might feel pain or discomfort in your scrotum – it may feel like a pulling sensation or heavy feeling. Other testicular cancer symptoms can include a testicle that looks bigger than usual, or a dull ache or heavy feeling in your lower tummy.
See our symptoms of testicular cancer section for more information.
You may still be able to have children after testicular cancer. If you have one of your testicles removed, the remaining testicle will still make sperm. And it will make enough of the hormone testosterone. But chemotherapy and radiotherapy can lower your fertility. If you have both testicles removed, you’ll be unable to have children (infertile). If you want children, you may be able to bank your sperm.
Very few people get cancer in both testicles. But if you do, you’ll need to have both testicles removed. Your testicles make sperm and produce the hormone testosterone. So, if you have both testicles removed, you’ll be unable to have children. Your doctor will offer you the chance to bank your sperm, if you wish, and prescribe you testosterone replacement therapy.
Statistics suggest that the survival rate for testicular cancer is 95% after 5 years. This means around 9 in 10 people diagnosed with testicular cancer in England are alive 5 years or more later. Your survival will depend on things like your personal general health, what type of cancer you have and when you get treatment. Ask your doctor to explain this to you.
If your testicular cancer comes back, your doctor will offer you more treatment (usually chemotherapy), which might still cure your cancer. Surgery might also be necessary to remove lymph nodes in your tummy or if cancer has spread to other parts of your body, such as your lungs.
It’s important to attend follow-up hospital appointments after treatment for testicular cancer so your doctor can check whether your cancer has come back and offer you the best treatment.
See our after your treatment section for more information.
Other helpful websites
Male infertility
If your partner hasn’t got pregnant after a year of regular sex and no contraception, this could be a sign of fertility problems.
Did our Testicular cancer information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- What is testicular cancer? Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 February 2022
- Testicular cancer. BMJ Best Practice. Bestpractice.bmj.com, last reviewed 30 April 2023
- European Association of Urology guidelines: Testicular cancer. European Association of Urology. Uroweb.org, updated March 2023
- Scrotal pain and swelling. NICE Clinical Knowledge Summaries. Cks.nice.org.uk, last revised January 2022
- Testicular cancer. Medscape. Emedicine.medscape.com, updated 17 August 2021
- Undescended testes. NICE Clinical Knowledge Summaries. Cks.nice.org.uk, last revised February 2020
- Causes and risk factors of testicular cancer. Macmillan. www.macmillan.org.uk, reviewed 1 May 2022
- Testicular cancer symptoms. Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 February 2022
- Urology. Royal College of Surgeons of England. www.rcseng.ac.uk, accessed 31 May 2023
- Testicular cancer. Macmillan. www.macmillan.org.uk, reviewed 1 May 2022
- Removing a testicle (orchidectomy) for testicular cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 February 2022
- Testicular cancer, sex and fertility Macmillan. www.macmillan.org.uk, reviewed 1 May 2022
- Parekh NV, Lundy SD, Vij SC. Fertility considerations in men with testicular cancer. Transl Androl Urol 2020; 9(Suppl 1):S14–S23. doi: 10.21037/tau.2019.08.08
- Your sex life and testicular cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 February 2022
- Fertility after testicular cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 February 2022
- Survival for testicular cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 February 2022
- Cancer survival for common cancers. Cancer Research UK. www.cancerresearchuk.org, last reviewed 29 April 2014
- If your testicular cancer comes back. Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 February 2022



