Anal fistula surgery
Expert review by:
Mr Toby Hammond, Consultant Surgeon
Content review by:
Liz Woolf, Freelance Health Editor
Page last reviewed: May 2024
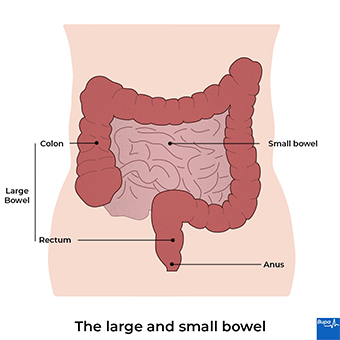
An anal fistula is an abnormal connection (like a small tunnel) between the inside of your anus and the outside skin of your bottom. The tunnel usually passes through some of the muscles that surround the anus (the anal sphincter). You’ll usually need to have surgery to treat an anal fistula.
About anal fistula
An anal fistula can develop after an infection of the anal glands. These glands sit between the muscles that surround the anus. The infection can cause an abscess (a collection of pus) in the gland. As this pus collects and drains, it forms a channel between the inside of the anus and the outside skin. This channel is the fistula. In around 3 out of 10 people, the drainage channel doesn’t heal and goes on to develop a fistula.
If the abscess doesn’t burst and drain by itself, it will need to be opened and drained in hospital.
Most fistulas aren’t related to any other medical condition. But they can also be caused by long-term bowel conditions such as Crohn’s disease. Anal fistula is more common in men than women. And it’s most common between the ages of 20 and 40.
An anal fistula is usually a single tunnel between your skin and your anal canal. But sometimes, other branches can develop off the main tunnel. Or the tunnel may pass through the muscles of your anus (your anal sphincter muscles). These are known as complex anal fistulas and can be more difficult to treat.
Anal fistula treatment is usually surgery. Anal fistulas don’t usually heal by themselves. Without treatment, they can lead to repeated abscesses.
Symptoms of anal fistula
Anal fistula symptoms can include:
- a hole or lump near the opening of your anus
- discharge from the opening of the fistula in your skin – this may have pus, blood or poo in it
- pain, discomfort and swelling in and around your anus
- irritated skin around your anus
These symptoms aren't always caused by an anal fistula but if you have them, see your GP.
Diagnosis of anal fistula
Your GP will ask about your symptoms and may examine you. Your GP may be able to see the opening of an anal fistula in the skin around your anus. They call this the external opening.
They may check for further signs by gently inserting their gloved finger into your anus. Your GP may send you to a colorectal surgeon for further investigation and treatment.
Your surgeon may need to do some more tests and examinations. You may need these if the diagnosis isn’t clear or if you have a complex fistula with multiple tracts.
These tests may include:
- an ultrasound scan using a probe that your surgeon will gently put up your anus
- a magnetic resonance imaging (MRI) scan
Your surgeon may also do a more detailed physical examination of your anus. You may have this done under general anaesthesia which means you’ll be asleep. Or you may have regional anaesthesia which means the lower part of your body will be numb.
Your surgeon may be able to treat you during this examination under anaesthesia (EUA). They’ll explain beforehand what they might do during your procedure.
About anal fistula surgery
There are several different types of surgery doctors use to treat an anal fistula. The aim of surgery is to remove the fistula but cause as little damage to the sphincter muscles around your anus as possible. These muscles allow you to control when you poo and pass wind. Depending on how much damage is caused, you may have less ability to hold on to wind and poo after the surgery.
After your surgeon has assessed you, they’ll talk to you about your treatment options. They’ll outline the risks and benefits of each and tell you what they recommend in your case. This will depend on:
- where exactly your fistula is
- whether it involves any of the sphincter muscle and if so, how much
Your surgeon will explain exactly what will happen during the procedure. they’ll tell you what to expect afterwards and the risk of potential complications. be sure to ask any questions you have and, if you need it, ask for more time to decide. if you’re happy to go ahead with the procedure, you’ll be asked to sign a consent form. it’s important to make sure you understand everything before you sign.
There’s more information in our section on types of anal fistula surgery.
Preparation for anal fistula surgery
Your surgeon will explain how to prepare for your anal fistula surgery. For example, if you smoke, they’ll ask you to stop. Smoking increases your risk of getting a wound or chest infection, and your wound won’t heal as well.
Your operation will usually be done under general anaesthesia, so you’ll be asleep. But some procedures for anal fistula can be done using regional anaesthesia. This means you’ll be awake during the operation, but the lower part of your body will be numb.
If you’re having a general anaesthetic, you’ll need to stop eating and drinking a few hours beforehand. In general, you can drink clear fluids (such as water, black tea or coffee) up until two hours before your anaesthetic. Follow the advice you get from your anaesthetist or doctor – if you have any questions, just ask.
On the day of your procedure, your surgeon will meet with you to check you’re well and still happy to go ahead. The staff at the hospital will do any final checks and get you ready for surgery. To help prevent deep vein thrombosis (DVT) you may need to wear compression stockings.16 Or you may have an injection of an anticlotting medicine. The DVT preventive measures you have will be specific to you and your surgeon will explain what you need.
Types of anal fistula surgery
Fistulotomy
The most common type of operation for fistulas is a fistulotomy. This involves opening up the fistula so that it can heal from the inside out.
Once your anaesthetic has taken effect, your surgeon will put a thin metal probe into the opening and along the fistula. This helps them to track the whole of the fistula. For most fistulas, they’ll then cut through your skin and along the length of the fistula. They’ll leave the wound open (they won’t use any stitches) so that it can gradually heal from the inside out.
This operation works well for most fistulas. But if your surgeon finds that you have a complex fistula, they may refer you to a specialist for a different type of treatment. In the meantime, they may treat your fistula with a ‘seton’. A seton is a length of thread. The surgeon lays the seton along the length of the fistula, from one end to the other. This won’t heal the fistula. But it helps it to drain and controls your symptoms until you can have further treatment.
Some people have long-term treatment with setons, without having any other procedures.6 This type of treatment is particularly used for people who have Crohn’s disease.6
Options for recurring and complex fistulas
You may need a different type of treatment if you have a fistula that keeps coming back. Or if you have a complex fistula, which means that either:
- your fistula passes through more of your sphincter muscle
- your fistula has more than one branch
Other types of surgery include the following.
- Anal advancement flaps
This approach avoids your surgeon needing to cut through your sphincter muscle. The surgeon creates a ‘flap’ of tissue within your anal canal. They then sew the flap over the internal fistula opening, to seal it. The fistula can then heal. - LIFT (ligation of the inter-sphincteric fistula tract)
Ligation means to tie off. This treatment is used for fistulas that pass through the sphincter muscles. It means the sphincter muscles don’t need to be cut. The surgeon closes up one end of the fistula. Then they find where the fistula passes between your sphincter muscles and tie it off there. - Endoscopic ablation or laser therapy
In endoscopic ablation, the surgeon passes a tiny camera and electrode along the fistula. The surgeon uses the electrode to burn away the tissue inside the fistula and seal it. - LAFT (laser ablation of the fistula tract)
Your surgeon may use a laser to destroy and seal the fistula in a similar way to endoscopic ablation.
There’s limited evidence on how well these therapies work.
Plugs, glues and pastes
The surgeon cleans out the fistula track and then uses a surgical glue or paste to block up your fistula. There isn’t much evidence to show that these work any better than other types of treatment. But they do avoid cutting your sphincter muscle.
Aftercare for anal fistula surgery
You’ll need to rest until the effects of the anaesthetic have passed. You’re likely to have some discomfort, so your hospital team will offer you pain relief. Once you’re ready, your nurses will encourage you to get up and move around. This will help to prevent complications. You can begin to drink and eat when you feel ready.
You’ll usually be able to go home on the day of your surgery. But ask someone to drive you home and stay with you overnight. Having a general anaesthetic can really take it out of you. You might find that you're not so co-ordinated or that it's difficult to think clearly. This should pass within 24 hours. During this time, you shouldn’t:
- drive or cook
- operate any dangerous equipment
- make any important decisions or post on social media
Before you go home, you’ll be given some advice about caring for your wounds. Your nurse will explain about signs of infection to look out for and pain relief you can take. You’ll also be told what the arrangements are for follow-up in the clinic.
Recovery after anal fistula surgery
You’re likely to have some discomfort for a week or so after anal fistula surgery. You can take over-the-counter painkillers such as paracetamol or ibuprofen. Constipation can be common after surgery. Your surgeon may recommend that you take a laxative to soften your poo and help to reduce any discomfort. Always read the patient information leaflet that comes with your medicine. If you have any questions, ask your pharmacist for advice.
Your wound should heal within a few weeks. Depending on the size of your wound, you may need daily visits to hospital or your GP practice to have your dressings changed. This helps to keep your wound clean and allow it to heal. Your surgeon will let you know how long you’ll need dressings for. You might find it helpful to put a gauze pad in your underwear for the first week or two. This will protect your clothes from any discharge from your wound.
Have a bath or shower two or three times a day to help ease pain and discomfort, as well as to keep your wound clean. Don’t add anything to the bath water as this may irritate your wound. Dry the area carefully afterwards.
You can probably get back to your usual activities and routine after a few days. Your surgeon will give you advice about driving, going back to work and having sex.
Complications of anal fistula surgery
Complications are when problems happen during or after the operation. Every operation has possible complications. These include infection, bleeding, and a reaction to the anaesthetic.
Specific complications of an anal fistula operation include the following.
- You may have trouble holding onto wind or poo, or have sudden urges to poo that are difficult to control. The risk of this happening is different for different types of procedure. Your surgeon will advise on the best type of operation in your case to minimise this risk.
- Your wound may take longer than usual to heal.
- The fistula may come back. The chance of this happening varies between different procedures. You may need a different type of operation if it comes back.
- As your fistula starts to heal, you may find it difficult to poo. Your doctor may suggest you take laxatives to help prevent this.
Sepsis (adults)
Sepsis is a life-threatening complication that can develop if you get an infection. Sepsis is a medical emergency. Call 999 or go to A&E immediately if you have any of the following symptoms:
- slurred speech, confusion, difficulty making sense
- extreme shivering or muscle pain
- passing no pee (urine) during a day
- severe difficulty breathing, feeling breathless or breathing very fast
- a feeling of doom or sudden acute fear of dying
- blue, pale or blotchy skin, or a rash that does not fade when you roll a glass over it
An anal fissure is a tear in the lining of your anus. Treatment for a fissure is to keep the area clean and make sure that your poo is soft and easy to pass while the fissure heals. An anal fistula is a tunnel that runs from your rectum out to the skin near your anus. You usually need an operation to repair it.
Generally, fistula surgery is not major. You can usually go home the same day. There are different types of surgery. Your surgeon will advise on which is the best in your case.
For more information, see our section on types of anal fistula surgery.
Generally speaking, fistula surgery isn’t urgent. But this depends on your circumstances and symptoms. If you have an abscess and are very unwell, it may need to be done more quickly.
For more information, see our section about fistula surgery.
It usually takes about a week or so for you to feel better and for any discomfort to go away. And your wound should heal within a few weeks. Your surgeon will give you advice about getting back to your usual routine. This is usually after a few days.
For more information, see our section on recovery after anal fistula surgery.
You’re likely to have some discomfort for two or three weeks after anal fistula surgery. You can take over-the-counter painkillers such as paracetamol or ibuprofen if necessary.
For more information, see our section on recovery after anal fistula surgery for more information.
Did our Anal fistula surgery information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Fistula-in-ano. Medscape. emedicine.medscape.com, updated 27 March 2020
- Vogel JD, Johnson EK, Morris AM, et al. Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Dis Colon Rectum 2016; 59(12):1117–33. doi: 10.1097/DCR.0000000000000733
- Endoscopic ablation for an anal fistula. The condition, current treatments and procedure. National Institute for Health and Care Excellence (NICE). www.nice.org.uk/guidance/ipg645/chapter/2-The-condition-current-treatments-and-procedure, accessed published 17 April 2019
- Anorectal abscess. BMJ Best Practice. bestpractice.bmj.com, last reviewed 3 December 2021
- Gastrointestinal medicine. Oxford handbook of general practice. Oxford Medicine Online. oxfordmedicine.com, published online June 2020
- Anorectal disorders. Colorectal surgery. Oxford Medicine Online. oxfordmedicine.com, published online August 2021
- Anal fistulas. Guts UK. gutscharity.org.uk, accessed 3 January 2022
- Personal communication, Nick Reay-Jones, Consultant Surgeon, General Surgery, 9 February 2022
- Anaesthesia explained. Royal College of Anaesthetists. www.rcoa.ac.uk, published 1 March 2021
- Lee MJ, Heywood N, Adegbola S, et al. Systematic review of surgical interventions for Crohn's anal fistula. BJS Open 2017; 1(3):55–66. https://doi.org/10.1002/bjs5.13
- Preparing your body. Royal College of Anaesthetists. www.rcoa.ac.uk, accessed 3 January 2022
- Joint briefing: smoking and surgery. TRCOA Action on Smoking and Health, The Royal College of Surgeons of Edinburgh and the Faculty of Public Health. ash.org.uk, published April 2016
- Nottingham JM, Rentea RM. Anal fistulotomy. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 11 August 2021
- Bioprosthetic plug insertion for anal fistula. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 25 September 2019
- Collagen paste for closing an anal fistula. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 29 May 2019
- Endoscopic ablation for an anal fistula. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 17 April 2019
- Radially emitting laser fibre treatment of an anal fistula. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 13 March 2019
- Postoperative care. MSD Manual Professional version. www.msdmanuals.com, last full review/revision November 2020
- Anal abscess and fistula. Association of Coloproctology of Great Britain and Ireland. www.acpgbi.org.uk, accessed 4 January 2022
- You and your anaesthetic. Royal College of Anaesthetists. www.rcoa.ac.uk, published February 2020



