Anal fissure
- Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon
- Liz Woolf, Freelance Health Editor
Key points
- An anal fissure is a small tear in your back passage that can cause pain when you poo.
- Anal fissures are common. They’re often caused by hard or painful bowel movements, or pregnancy.
- Most anal fissures heal by themselves, but eating a high fibre diet to prevent constipation and taking certain medicines can help.
- If you’re in pain or have bleeding from your bottom you should seek medical help.
What is an anal fissure?
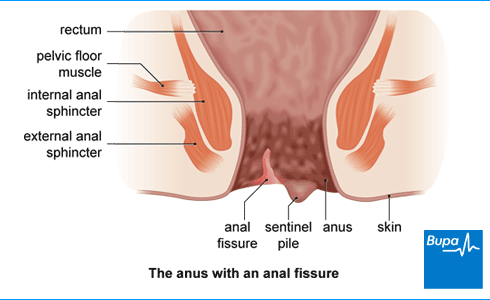
An anal fissure is a small tear or open sore (ulcer) in the skin just inside your anus (bottom or back passage). It causes pain and sometimes bleeding when you have a bowel movement (poo). Anal fissures are common and often go away by themselves. But if they don’t, there are treatments that can help.
Causes of anal fissure
The cause of anal fissure is often unknown, or you might be aware of certain factors that have caused it.
What is the main cause of anal fissure?
It’s often thought to be caused by hard or painful bowel movements. These can cause the muscles around your anus to tense up and spasm, making your anus more likely to tear. It also reduces the blood supply to the area, which makes it harder for any tears to heal.
Sometimes, there is a clear underlying cause for an anal fissure. These can include:
- constipation – a hard poo can cause a tear
- pregnancy or giving birth – this can put pressure on the area between the anus and vulva (your perineum)
- inflammatory bowel disease such as Crohn’s disease
- a sexually transmitted infection or a skin infection
- a skin condition such as psoriasis
- medicines that are constipating such as opioid painkillers or some chemotherapy drugs
- trauma to your anus – for example, through having anal sex or through surgery
- bowel cancer
Symptoms of anal fissure
If you have an anal fissure, you’re likely to experience symptoms that can be worse after a bowel movement.
What does an anal fissure feel like?
With an anal fissure, you may feel a tearing sensation when you poo.
Once you have a tear in your anus, it can cause:
- pain when you poo - this may be sharp, searing, or burning pain in or around your bottom
- a deep, burning pain for several hours after you poo
- bleeding from your anus – you might see blood in the toilet or on the toilet paper after you’ve had a poo
- spasms (sudden tightening) in the muscles around your anus when you poo
These symptoms may not always be due to an anal fissure. Other conditions, like piles (haemorrhoids) can cause similar symptoms. If you have any of the symptoms above, contact a GP for advice. You should always seek medical advice if you notice bleeding from your bottom.
Looking for prompt access to quality care?
You could access specialist support teams to guide you through treatment that may occur.
To get a quote or to make an enquiry, call us on 0808 273 6216∧
Diagnosis of anal fissure
A GP will usually be able to diagnose an anal fissure by asking about your symptoms and examining you.
A doctor may:
- examine you by asking you to lie on your side with your knees bent towards your chest
- gently part your buttocks to examine the area and see if there’s a fissure
If there’s uncertainty about what’s causing your symptoms or if initial treatments don’t help, your GP may refer you to a colorectal surgeon. This is a surgeon who specialises in conditions affecting your bowel and back passage.
What should I do if I'm embarrassed to talk to my doctor?
Seeing a doctor when you're embarrassed | Watch in 2:08 minutes
Dr Naveen Puri talks about how to make it easier to see a doctor about a health issue when you are feeling embarrassed.
Hello, I am Dr Naveen Puri, I am one of the GPs within Bupa Health Clinics.
Today I want to speak to you about embarrassing problems you might have and what we can do if you attend one of our clinics.
I want you to know that many people feel embarrassed or concerned about speaking about certain things with their doctors, but I'm here to reassure you these are the kinds of things we deal with every day.
For me, looking at someone's bottom or their breasts or their genitalia is no different to looking at their nose or elbow.
And that's true for all doctors as we train for many years in these parts of the body and are very used to having these conversations with people just like you.
So what I would encourage you to do if you have any concerns from your perspective, be it a change in your bowel habit, be it a lump, a rash, a swelling. Something on your genitalia or a part of your body you're not particularly familiar with or feel uncomfortable discussing.
Please be assured your doctor has done it all before.
Some of the ways we find patients find it easier to speak to a doctor is to either tell the doctor you feel embarrassed up front. That way a doctor can make extra effort to make sure you feel comfortable.
Or some patients come to us with pieces of paper and will write the problem down and hand it to us. That way we can help with whatever is going on for you as well.
You may also find it helpful to ask for a specific doctor, someone you're familiar with in your practice. Or you might want to ask for a doctor of a specific gender, or background to your liking as well.
I'd also say, doctors do this every day so don't be alarmed if we ask you certain questions around your symptoms. It is purely so we can help you get the best outcome for your enquiry.
And then finally, feel free to use language that suits you as well. We don't expect you to know the medical words for things, or a name for your diagnosis. That's our job to find out for you.
So, take your time, see a doctor, and hopefully we can help put your mind at ease.
Self-help
There are certain things you can do to ease your symptoms and help your anal fissure to heal.
How do you know if an anal fissure is healing?
Most anal fissures heal by themselves within six to eight weeks.
As your fissure is healing, your pain should lessen, and any bleeding should stop. You should have a follow-up appointment with your doctor after six to eight weeks, to check that the fissure has healed.
How do you heal an anal fissure?
Your anal fissure should heal by itself, but the following tips may help.
Eating and drinking
Gradually increase the fibre in your diet as this will help keep your poo soft and easier to pass. You should aim for up to 30g per day in total. You can get fibre from wholegrain foods, fruit, and vegetables. You should also make sure you’re drinking enough fluids.
Staying regular
Because of the pain, you may tend to delay going for a poo. But make sure you go to the toilet as soon as you feel the need and try not to strain when you go, as this can make the fissure worse.
Hygiene and comfort
Keeping the area clean and dry is important to help with healing and prevent infection. Sitting in a warm bath after you’ve had a bowel movement may help to relieve any pain.
You can also manage pain with over-the-counter painkillers such as paracetamol or ibuprofen. Make sure you read the patient information leaflet in the packet.
Treatment of anal fissure
If your pain is severe or your symptoms aren’t improving, there are a number of treatments your doctor may suggest.
Medicines
There are several different types of medicine that can help to relieve pain or help the fissure to heal.
Laxatives or stool softeners
Ispaghula husk or lactulose can help if you’re constipated. These work by softening your poo and making it easier to pass. You can buy laxatives over the counter from a pharmacy. A doctor will need to prescribe them if they are for a child.
Anaesthetic ointment
Your GP may prescribe an anaesthetic ointment (for example, lidocaine) to help with pain when you poo. You apply this ointment to your anus to help numb the area before you have a bowel movement.
Glyceryl trinitrate (GTN) ointment
Your doctor may also suggest an ointment containing glyceryl trinitrate (GTN). This helps to relax the muscles in your anus and improve blood flow to the area, which helps the fissure to heal. You’ll need to keep using it for six to eight weeks.
GTN ointment isn’t suitable for children or pregnant women.
Calcium-channel blockers
A cream containing calcium-channel blockers (for example, diltiazem cream) also relaxes the muscles and improves blood flow to the area. It has fewer side-effects than GTN ointment.
Procedures to treat anal fissure
If other treatment options haven’t helped your anal fissure to heal or it keeps coming back, your GP may refer you to a colorectal surgeon. Your surgeon may discuss other options with you. These include the following.
- Botox injections into the sphincter muscle in your bottom. The aim is to temporarily relax this muscle so that your fissure can heal.
- Lateral internal sphincterotomy – a type of surgery that involves cutting the sphincter muscles in your anus. This releases the tension around your anus and lets your fissure heal.
- Fissurectomy – cutting away the damaged skin around your anal fissure.
- Anal advancement flaps – taking healthy skin from your anal lining and using it to replace the broken skin in your fissure.
There is more information about these procedures in our page of information on anal fissure procedures.
Prevention of anal fissure
You can reduce your risk of developing an anal fissure by preventing constipation.
A healthy balanced diet that contains plenty of fibre can help. It’s also important to make sure you’re drinking enough fluids and exercising regularly.
If you have another health condition that increases your risk of getting an anal fissure, speak to your doctor. They will tell you the best way to manage your condition and reduce your risk.
Anal fissure procedures
If you have an anal fissure that hasn’t healed with other treatments, your doctor may suggest surgery.
Constipation
Constipation is a common condition that affects your usual pattern of bowel movements.
Why is fibre important?
Fibre is a plant-based carbohydrate found in foods such as wholegrains and vegetables, also described as roughage. Many of us don’t get enough fibre in our diets.
Piles
Did our Anal fissure information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Anal fissure. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2021
- Anal fissure. BMJ Best Practice. bestpractice.bmj.com, last reviewed July 2023
- Anal fissure clinical presentation. Medscape. emedicine.medscape.com, last updated March 2023
- Anal fissure. Patient. patient.info, last updated October 2022
- Suspected cancer: recognition and referral. National Institute for Health and Care Excellence (NICE). nice.org.uk, last updated January 2021
- Fibre: food fact sheet. British Dietetic Association. www.bda.uk.com, published April 2021
- Oxford Handbook of General Practice (5th edit). Oxford Academic. academic.oup.com, published online June 2020
- Constipation in children. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised November 2020
- Colorectal Surgery (2nd edit). Oxford Academic. academic.oup.com, published online July 2021
- Anal fissure treatment & management. Medscape. emedicine.medscape.com, last updated March 2023
- Constipation in adults. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised January 2023



