Bowel surgery
Your health expert: Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon
Content editor review by Rachael Mayfield-Blake, April 2023
Next review due April 2026
There are lots of types of bowel surgery. This information is about surgery to remove all or part of your large bowel (colon). This is called a bowel resection. You might need this type of surgery if you have a bowel condition such as bowel cancer, diverticular disease, Crohn’s disease or ulcerative colitis.
About bowel surgery
There are different types of bowel surgery. The exact procedure you have will depend on:
- the reason why you need surgery
- if you need to have all or part of your bowel removed – how much of your bowel is affected.
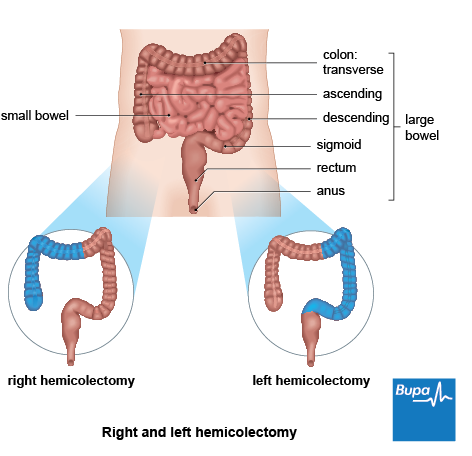
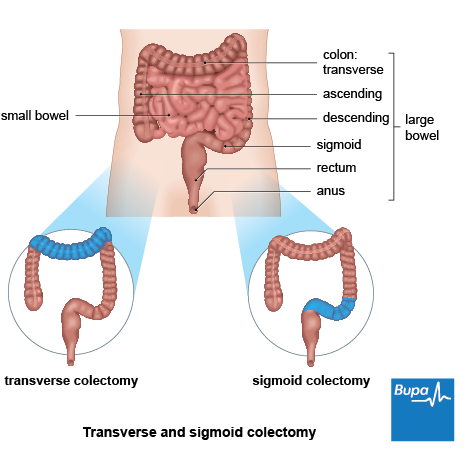
The procedures to remove part of or all your bowel are named by what section of bowel is removed and include:
- total colectomy – all of your large bowel is removed
- proctocolectomy – your large bowel and back passage (rectum) are removed
- panproctocolectomy – your large bowel, anus and back passage are removed
- hemicolectomy – either the left or right side of your large bowel is removed
- sigmoid colectomy – the part of your bowel that’s closest to your back passage is removed
- transverse colectomy – the middle part of your large bowel is removed
- proctectomy – all or part of your back passage is removed
Your surgeon will explain what the most appropriate procedure is for you.
Preparation for bowel surgery
Your doctor will discuss your surgery with you and explain what will happen before, during and after your procedure. They will also explain the risks and benefits. Ask your doctor if you have any questions or need a more detailed explanation. You’ll be asked to sign a consent form before the procedure, so it’s important that you understand.
Getting ready for surgery
You’ll be assessed before your operation to check that you’re fit for surgery. This may happen at a preoperative assessment clinic when they’ll also explain how to prepare for your operation.
You may need to take laxatives on the day of your surgery or the night before, to clear out your bowel. Or you may need to have an enema. This is when a small amount of liquid medicine is inserted into your back passage (rectum) to help you empty your bowel.
You’ll usually need to stay in hospital between three and 10 days for bowel surgery, so make any necessary preparations for this.
On the day
You’ll have bowel resection surgery under general anaesthesia, which means you’ll be asleep during your operation. Your hospital team will give you instructions about when to stop eating and drinking before your anaesthetic. You may be given a carbohydrate-rich drink to have the night before your surgery and again a few hours beforehand.
When you come into hospital, one of the team will talk you through what will happen and answer any questions. They’ll check that you’re well and still happy to go ahead. They may give you some compression stockings to wear and also give you an injection of an anti-clotting medicine called heparin. This helps to prevent blood clots forming in the veins in your legs. You may also have an antibiotic injection before your operation to reduce your risk of infection.
Bowel surgery
In bowel resection surgery, your surgeon will remove the diseased parts of your bowel and, if possible, join the two healthy ends together. They’ll use stitches or staples, and this is called an anastomosis.
Sometimes, your surgeon may need to bring the healthy end of your bowel through your tummy (abdominal) wall and onto the surface of your skin. This is called a stoma. If the operation involves your large bowel, it’s called a colostomy; if it involves your small bowel, it’s called an ileostomy. The waste from your bowel will pass out of the stoma, and collect in a bag that you wear over the stoma. A stoma can either be temporary or permanent, depending on the type of surgery you have and how much bowel your surgeon removes.
If your surgeon thinks you may need a stoma, they’ll arrange for you to see a specialist stoma nurse before your operation.
If you’re having a proctocolectomy to remove all your large bowel and back passage, your surgeon may create a ‘pouch’ from the end of your small bowel. This can store the waste from your bowel and allow you to pass poo through your anus.
Keyhole and open bowel surgery
There are two main ways you can have bowel surgery: keyhole (laparoscopic) and open surgery.
- In keyhole surgery, your surgeon will insert instruments and a tube-like telescopic camera through small cuts in your tummy (abdomen). They then remove a section of bowel through a larger cut. Images from the camera are shown on a monitor so your surgeon can see what they’re doing.
- In open surgery, your surgeon will make a single, large cut into your tummy to reach your bowel and remove the affected section.
People often (but not always) recover more quickly from keyhole surgery, don’t have to stay in hospital for so long and may have less pain afterwards. Not everyone can have keyhole surgery though – ask your surgeon if it’s an option for you. Sometimes your surgeon will need to switch from keyhole to open surgery during the operation. They’ll talk to you about the possibility of this happening and what it will mean, before your surgery.
Robotic surgery
Robotic surgery uses robotics for surgery on the back passage (rectum). The robotic machine has several arms – one holds the camera, and the others hold surgical instruments. Your surgeon will control the arms of the machine to operate on you.
This is a relatively new technique, so it’s not available in all hospitals. It’s still being investigated to understand how it compares to open and keyhole surgery.
Aftercare for bowel surgery
You’ll spend the first few hours after your operation in a recovery unit, before you’re transferred to a ward or other unit. You might have some discomfort as the anaesthetic wears off, but you’ll be offered pain relief as you need it. This will often be patient-controlled analgesia or an epidural. In patient-controlled analgesia, morphine is delivered directly into a cannula or drip. In an epidural, pain-relieving medicine is delivered into the space that surrounds your spinal cord (the epidural space).
At first, you’ll have a catheter to drain pee (urine) from your bladder into a bag. You may also have fine tubes (drains) running out from your tummy to drain fluid into another bag for a few days. You’ll have a drip in your hand or arm to give you fluids for a day or so. Your hospital team will encourage you to eat and drink as soon as you feel ready. Read our FAQ on what to eat after bowel surgery for more information.
To help prevent deep vein thrombosis (DVT), you’ll have a daily injection of an anti-clotting medicine and will need to keep wearing compression stockings. Try to get out of bed and move around as soon as possible. A physiotherapist or nurse may show you some exercises you can do while you sit or lie down, including breathing exercises to clear your lungs.
When you can go home after surgery will depend on the type of surgery you had, and your recovery. If you had surgery to treat bowel cancer, you’ll usually go home about a week later. If you had surgery to treat Crohn’s disease it can vary between individuals. Before you go home, your nurse will give you some advice on how to care for your healing wounds and stoma if you have one.
Recovery for bowel surgery
It can take weeks to recover after bowel surgery. Don’t lift anything heavy or do any strenuous exercise for at least six weeks – ask your surgeon how long.
It’s normal to feel tired while you recover and to need to sleep and rest more than usual. It’s important to take time to rest. But do try to get up and move around as much as you can, and keep up any exercises your physiotherapist gave you. This can help you to feel better and get your strength back as well as reduce your risk of complications.
Looking for prompt access to quality care?
With our health insurance, if you develop new conditions in the future, you could get the help you need as quickly as possible, from treatment through to aftercare.
To get a quote or to make an enquiry, call us on 0800 600 500∧
Complications of bowel surgery
Complications of bowel surgery include the following.
- The new join in your bowel may leak (an anastomotic leak). This can cause severe tummy (abdominal) pain, and you may feel very unwell with a high temperature. You may need to go into hospital for further treatment and surgery.
- A wound infection. Your wound may become swollen, red and tender to touch. You might have a high temperature too, and feel sick. Contact your hospital if you develop these symptoms.
- Bands of scar tissue (adhesions). These can develop after surgery and may cause your tissues or organs to stick together. This can cause ongoing pain in your tummy. Adhesions can also block your bowel. You might be able to have a procedure to break them up.
- Temporary paralysis of your bowel (ileus). It takes time for your bowel to start working again properly. You may feel bloated, be sick or have problems with your bowel movements. If this doesn’t get any better after a few days, your hospital team will give you fluids to help you recover.
- Nerve damage. If nerves in your rectum are damaged during surgery, it can affect your sex life or how well you can control your bladder. For more information, see our FAQ on bowel surgery and sex.
Sepsis (adults)
Sepsis is a life-threatening complication that can develop if you get an infection. Call 999 or go to A&E immediately if you have any of the following symptoms.
- Slurred speech, confusion, difficulty making sense.
- Extreme shivering or muscle pain.
- Passing no pee (urine) during a day.
- Severe difficulty breathing, feeling breathless or breathing very fast.
- It feels like you’re going to die.
- Skin changes, such as your skin looking blue, pale or blotchy, or a rash that doesn’t fade when you roll a glass over it.
Yes, you’ll usually need to change what you eat while you recover from bowel surgery. Eating low-fibre food, such as white bread and well-cooked or peeled fruit and vegetables can help to prevent diarrhoea. Avoid foods and drinks that may cause bloating and wind, such as beans and fizzy drinks. And try to eat smaller, more frequent meals, high in calories and protein. As your bowel heals, you will be able to eat more. Your hospital will give you more advice.
Bowel surgery may affect your sex life. If you have surgery near your back passage (rectum), it may affect your pelvic nerves, which can lead to difficulties when you have sex. Problems include erection or ejaculation problems, and reduced sensitivity and changes to the vagina, which might make sex painful. Talk to your doctor or nurse if this is affecting you because they may be able to help.
Having a colostomy or ileostomy bag shouldn’t stop you doing any of the things you used to do. But it can take time to get used to it and you may need to make some adjustments and plan ahead more. You can bath or shower with one on, and you can get a device to stop your seat belt pressing on your stoma and bag when you drive. Colostomy and ileostomy bags shouldn’t leak or smell (except when you change them, and you can buy products to reduce this). There’s plenty of support – see our section on other helpful websites for details.
It can take weeks to recover from bowel surgery. You’ll likely feel tired to begin with while you recover and it’s important to take time to rest. But do try to get up and move around as much as you can because it will make you feel better and lower your chance of getting complications.
For more information, see our section on recovery for bowel surgery.
There are different types of bowel surgery to remove different amounts and sections of bowel. If you have a total colectomy, for example, all of your large bowel is removed, but if you have a transverse colectomy, only the middle part is removed. Your surgeon will explain what the most appropriate procedure is for you.
For more information, see our section: About bowel surgery.
How long you stay in hospital after bowel surgery will depend on the type of surgery you had, and how your recovery goes. If you had surgery to treat bowel cancer, you’ll usually go home about a week later. If you had surgery to treat Crohn’s disease, the time can vary a lot between individuals.
For more information, see our section on aftercare for bowel surgery.
Bowel cancer
Bowel cancer (or colorectal cancer) is the name for any cancer that starts in your large bowel, rectum (back passage) or appendix.
Did our Bowel surgery information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Colon resection. Medscape. emedicine.medscape.com, updated 5 April 2021
- Colorectal cancer. BMJ Best Practice. bestpractice.bmj.com, last reviewed 26 January 2023
- Your operation. A guide to bowel cancer surgery. Bowel Cancer UK. bowelcancer.org.uk, published July 2022
- Bowel resection. Canadian Cancer Society. cancer.ca, last reviewed 27 February 2023
- Anaesthesia explained. Royal College of Anaesthetists. www.rcoa.ac.uk, published 1 March 2021
- Radiotherapy for rectal cancer. Macmillan. www.macmillan.org.uk, reviewed 30 April 2020
- Venous thromboembolism in over 16s: Reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 13 August 2019
- Colon resection. Lieske B, Ahmad H. StatPearls publishing. www.ncbi.nlm.nih.gov, last updated 8 August 2022
- Types of surgery for colon cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 2 February 2022
- Colorectal cancer. National Institute for Health and Care Excellence (NICE). nice.org.uk, last updated 15 December 2021
- Epidural pain relief after surgery. Royal College of Anaesthetists. rcoa.ac.uk, published February 2020
- After surgery for bowel cancer. Cancer Research UK. cancerresearchuk.org, last reviewed 3 February 2022
- Surgery for Crohn's disease. Crohn's and Colitis UK. crohnsandcolitis.org.uk, last reviewed October 2022
- Personal communication, Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon, 21 March 2023
- Problems after surgery. Cancer Research UK. cancerresearchuk.org, last reviewed 4 February 2022
- Spinelli A, Bonovas S, Burisch J, et al. ECCO guidelines on therapeutics in ulcerative colitis: surgical treatment. J Crohns Colitis 2022; 16(2):179–89. doi: https://doi.org/10.1093/ecco-jcc/jjab177
- Laparoscopic adhesiolysis. Medscape. emedicine.medscape.com, updated 29 November 2022
- Postoperative ileus. Buchanan L, Tuma F. StatPearls publishing. ncbi.nlm.nih.gov, last update 1 August 2022
- Septic shock. Medscape. emedicine.medscape.com, updated 10 October 2020
- Fibre: Food fact sheet. British Dietetic Association. bda.uk.com, published April 2021
- Your sex life and bowel cancer. Cancer Research UK. cancerresearchuk.org, last reviewed 31 March 2022
- Living with a stoma. Colostomy UK. colostomyuk.org, published July 2021



