Bowel cancer
- Dr Haney Youssef, Consultant Colorectal and Peritoneal Surgeon
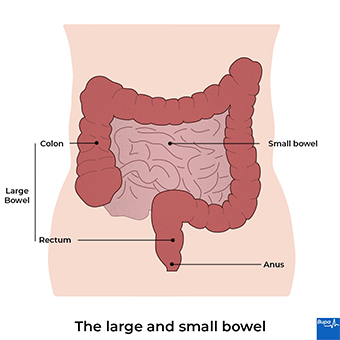
Bowel cancer is cancer that starts in your large bowel (colon) or inside your back passage (rectum). Other names for bowel cancer include colon cancer, rectal cancer, and colorectal cancer. Bowel cancer is one of the most common types of cancer in the UK; more than 40,000 people get bowel cancer each year.
Inside Health: Bowel Cancer
Bowel cancer| Symptoms | Screening |Diagnosis | Watch in 12:51 minutes
Dr Zoe Williams talks to bowel cancer surgeon Mr. Shahnawaz Rasheed about bowel cancer. They discuss how common it is, symptoms, screening for signs of bowel cancer and how to reduce risk of bowel cancer.
Thank you for joining us today, I'm joined by Mr. Shahnawaz Rasheed, who is a bowel cancer surgeon and we're gonna be having a conversation about all things bowel cancer.
So welcome.
First question.
What do we actually mean by bowel cancer?
So the bowels are the whole intestines which go all the way, really from the mouth to the bottom.
But when we talk about bowel cancer, we really talk about colon and rectum cancer.
Sometimes we say Colorectal cancer.
Exactly, that's the large intestine.
So the small intestines, the bit where you absorb the goodness of the food and the large intestines main job is to really absorb water.
So we don't get dehydrated, but also some vitamins to keep us healthy.
So when they talk about bowel cancer, really what they mean is colorectal cancer.
Okay. Great.
And how many people does bowel cancer affect here in the UK?
The numbers are increasing, but actually, it' s about 42,000 people per year Is that 42,000 people each year Who get it, who get bowel cancer and then about a third of those are rectum and the rest of them are the remainder of the colon.
Right, okay. So it's fairly common then as far as cancers go.
It's common. I mean, they talk about one in 15 men and one an 18 women in the whole population.
So it's, you know, one of the common cancers. In fact, is the fourth commonest cancer, but it results in the second largest number of deaths because lung cancer is commoner and it also causes deaths. Whereas prostate and breast are more common but they don't result in deaths as frequently.
And other some people that are more at risk more susceptible to getting bowel cancer than others?
Yeah, about a third of people have got a genetic link to it so they've got a relation who's got polyps or cancers and 70% of people just get it by itself.
Although it does cause some genetic abnormality.
It's not an inherited one.
And I think something that's important for us all to know is what are the typical signs and symptoms that we can look out for?
The commonest ones, commonest two are bleeding from the bottom and change your bowel habit and that normally means either more loose or more frequent.
So people often think it's constipation, I'm bit constipated and that means I’ve got bowel cancer, it's actually the opposite, It's actually looser and it's actually more frequent.
So if that remains for a period of time, obviously, we gone out for a night out and we've had a curry the night before, we're not talking about that we're talking about a sustained period of time where your bowels just become a little bit looser.
And there are other there are other symptoms, you can get bloating, you can feel abdominal pain, you can pass mucus from your button, but the two commonest things, bleeding from your bottom and change your bowel habit towards looseness.
And how important is it to tackle these signs early?
So if anybody is noticing that they're having these symptoms, how quickly should they act really, It's really, really vital.
The earlier you pick up on these things, the better your outcome will be.
Every single time.
So what we know is that bowel cancer, colorectal cancer starts off life as a polyp.
So it goes from normal bowel to polyp to cancer and there's a period of time between those different steps.
So if we can pick up something at the stage where it hasn't become cancerous and it's a benign polyp, then will prevent the cancer happening completely.
But even if it has become cancer, then the earlier you pick it up the earlier you deal with it, the better the outcome, you know, always.
So the difference between a benign polyp and a cancer is two things.
One thing is the ability of that thing to invade deeply into where it started off life and the second bit of it is the ability to spread elsewhere.
So those two features are what defines cancer but the benign polyp hasn't invaded.
So if you can just remove it as it is it doesn't become cancerous.
And where you get the cancers is the inner lining of the bowel wall, the very inner most lining, and that's the lining where glands are and the glands make mucus.
And so you have the change from normal to polyp and that creates the mucus and that makes your bowel looser on the whole.
So the polyp has got the similar symptoms to the cancer.
In this country, we do have screening available for bowel cancer, which is really good news because that is another tool to help us identify changes early on.
Can you tell us a little bit about the screening?
The screening is normally every two years for everyone in this country from the age of 60 onwards.
Many people are offered it at 56 as well in most areas and you have it every two years.
And what that does, it's not a test for cancer, but it's a test for the presence of blood in your poo.
That's an important thing to recognise because even if it comes back positive, the vast majority of people with a positive test doesn't mean they've got cancer.
It just means there's blood in the poo.
Now remember, the commonest cause for blood in the pool isn't cancer is haemorrhoids and other things in the bottom.
So although people might think.
Oh, I've just got haemorrhoids, with bleeding, you might be right.
But you want to be sure and you want to make sure that there's nothing else worse than that and so that's why we encourage the test to happen.
Now the new test, something called a FIT, which is stands for Faecal Immunochemical Test is a really accurate way of picking up the presence of microscopic blood in the poo.
So remember when we're looking at the picture, sometimes you don't see it looks normal, you know, some people look at their poo more than others as we know.
But people generally might not see anything, but the test will pick it up at a very sensitive level.
If it comes above a certain level and we that number is 10 above 10, then we would want to investigate with something like a colonoscopy or something like that.
And I wonder what your thoughts are as a GP, I sometimes will ask patients about their poo, particularly, you know, have you had a change of bowel habit?
Have you noticed any blood in your stool?
And often patients will say, Well, I don't look at my poo and almost seem quite embarrassed.
We need to change that, don't we?
Because we need to look at our poo.
I mean generally people are quite embarrassed to talk about these things aren't there I mean who wants to talk about their toilet habits.
Nobody does, really and so I think to raise that awareness is particularly important.
And particularly in younger people, I must say, something like 6% of people with colorectal cancer are under the age of 50.
So I think raising that awareness in all generations is really, really important isn't to say.
People justify the symptoms to themselves.
They say, oh it's this, it's that or hey it's something funny and all sorts of things that you've heard hundreds of times before thousands of times before, as I have, that you're just you justify it, because you don't want it to be those things.
So you make up something Oh, it's because I had something funny to eat, or I've got piles, or you say all these things, but actually having that awareness to say.
You know what, I can't look at somebody and say you've got bowel cancer, you know, none of us can.
So what we have to do is say, well, there's an index of suspicion you might have it you might not, but it's definitely worth investigating and finding out whether you do or not.
And the really important reason why is well, if it's not bowel cancer, that's reassuring, you don't have to worry about it anymore.
But if it is, finding it early means the chances of curing it essentially, are so much higher than if you you know, leave it for months to get worse.
Definitely and people say that to me that Explain to people, it's not that bad, the whole process of diagnosis of coming to the answer.
People are very scared of being examined or having tests that might be they might perceive to be difficult, or painful.
But if we can, I suppose make them feel more at home with us as clinicians and don't feel we break down those barriers between us.
I think that's really important.
Generally not just for bowel cancer.
I agree, coming back to screening.
I've actually got one of the little tests here.
I thought it might be quite nice to demonstrate just how easy this is to do.
So these if you're eligible for screening, and then people receive one of these in the post, and it's so simple.
All you do is when you've had poo in the toilet before you flush the toilet, take out this little stick and the end of it.
You just get a little bit of poo on the end of it Put it in there, flush the loo, Put it in an envelope, send it off.
And that's a screening test done.
But it surprises me, I'm looking at statistics here, it says just over half of people, and 58% in England and 56% in Wales, who received the screening test, complete it.
I look at that number. I think that's very low.
Remember people if they haven't got symptoms they'll think that's not for me, I'm alright. Thank you.
It's any when people have symptoms, they start seeking medical advice.
You're talking about people who are asymptomatic.
Yeah, On the whole aren't you so people who might have blood on their poop without realising it.
But they've got no change of their bowel habit.
They've got no pain, their alright.
So what most people think is if it ain't broke, don't try and fix me.
I'm alright. Thank you.
I think that's an important distinction to make isn't it?
Screening tests like this are designed for people who don't have symptoms to try and pick up in this case, any blood in the poo.
At such an early stage before it's even given symptoms.
So if people do have symptoms, don't hang around waiting for this, go and see a doctor straightaway.
This is not the test Exactly so if you have bleeding and you’ve seen it.
That trumps this, because you’ve actually seen blood.
What are the risks then of delaying, going to see a doctor in terms of I mean, I think the nitty gritty is survival.
So the earlier you pick up something, the better the outcome across the board.
if you pick up something in the polyp stage before it becomes cancerous, you just won't get cancer.
So you'll have 100% survival.
As you go further along that point, and we talked about stage a stage means a how bad it is or how advanced it is, or how spread it is.
So the further you are on your stage, the worst your outcome is going to be.
And that's purely time, a lot of the time.
So the longer you leave it, the thing might be growing invading and starting to spread.
So it's sort of it's sort of obvious that the further you leave something, the worse it gets.
And remember bowel cancer is one of the most treatable of all cancers.
And it's preventable, because you can pick it up before it becomes cancerous.
So some some cancers, they become so advanced so quickly, before any symptoms come and by the time They are hidden inside the body and they don’t you know have bleeding for example into the poo.
How is bowel cancer diagnosed?
First thing is somebody seeking medical advice, seeing primary care doctor, GP, and then getting referred to a specialist for further tests and the two sort of commonest test are a specialist kind of a CT scan called a virtual colonoscopy or a colonoscopy.
The colonoscopy means a tube up bottom, which looks and can identify and remove polyps and also see potential cancers for biopsy.
A CT scan can identify things bigger than about 4 or 5 millimeters but obviously can't remove them, or test them as it were.
So that the, the gold standard has a colonoscopy.
But if people really don't want to colonoscopy, they can have an alternative, which is a CT scan.
And we've spoken about how bowel cancer is actually quite common.
It's the fourth most common cancer.
So really, we're all potentially at risk.
So what can we all do to prevent or reduce our risk of getting it?
I suppose it’s a healthy lifestyle, reduction of smoking, drinking less alcohol, more activity trying to lose weight if you've put on a bit of weight.
And having a general awareness that you may have bowel cancer and seeking advice early. It's the same advice that I’d give to anyone in general really. The only additional thing was fibre in the diet and having more fruit, vegetables, those things are known to have a reduction in bowel cancer.
There's some evidence which is relatively weak, but red meats can increase your chance of bowel cancer, so wouldn't have red meat every day.
I mean, if you need to eat red meat, have it slightly more sparingly.
Okay. So I think that's really interesting.
That was you can't change your genetics.
You can't be more vigilant if you think you're at higher risk.
And then there's some healthy living things that that we can all do.
Shahnawaz, thank you so much for joining us.
I hope you found that as informative, interesting and useful as I did, and we'll see you again next time.
About bowel cancer
If you have bowel cancer, cells in your large bowel (colon) or back passage (rectum) start growing out of control. Most bowel cancers (around seven in 10) start in the colon, while around three in 10 start in the rectum. They usually develop from small, non-cancerous (benign) growths of tissue called polyps, which can become cancerous (malignant) over time.
Bowel cancer can spread through the wall of your bowel to the surrounding tissues, and to your lymph nodes nearby. It can also spread to other parts of your body, such as your liver and your lungs. The earlier bowel cancer is diagnosed, the better your chance of surviving it. So it’s important to see a GP if you have symptoms, and to consider screening tests if you’re offered them.
Causes of bowel cancer
It’s not known exactly what causes bowel cancer. It probably happens because of a mixture of different things.
Although you can develop bowel cancer at any age, it’s rare before 40. You’re more likely to get it as you get older. Your risk of developing bowel cancer is also higher if you:
- have a family history of bowel cancer – you’re more likely to get it if your brother, sister, or one of your parents has it
- have an inherited bowel condition, such as familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (HNPCC), also known as Lynch syndrome
- have a long-term bowel condition, such as Crohn's disease or ulcerative colitis
- have a history of non-cancerous growths (called polyps or adenomas) or previous cancers in your bowel
If you have any of these ‘risk factors’, your doctor may recommend you go for regular bowel cancer screening. See our prevention section for more information.
Other things that can increase your risk of bowel cancer include:
- obesity
- not eating enough fibre and/or eating a lot of processed and red meats
- not getting enough exercise
- type 2 diabetes
- smoking
- drinking a lot of alcohol
If you have any of these risk factors, it doesn’t mean you’ll definitely get bowel cancer – but they increase your chances of developing it. But you can develop bowel cancer without having any of them.
How cancer develops
Cancer explained | Watch in 1:48 minutes
In this video, we explain how, when cells divide uncontrollably, this leads to cancer.
Symptoms of bowel cancer
People don’t always get bowel cancer symptoms in the earlier stages. If you do, symptoms of bowel cancer can include the following.
- Bleeding from your bottom or blood in your poo may be one of the first signs of bowel cancer. The blood can be bright or dark red on the surface or mixed in with the poo. Or you may notice it in the toilet bowl. Occasionally it can make your poo look black, like tar.
- Changes in your bowel habits. Your poo may be looser (diarrhoea) or you may find it harder to go (constipation). You may feel like you need to go more often or more urgently or you might feel like you haven’t finished even when you’ve just been.
- You might feel extremely tired and weak (fatigued). This can be due to anaemia, which means you have a lower than normal level of red blood cells.
- Pain or discomfort in your tummy (abdomen) or back passage that doesn’t go away.
- Losing weight, when you haven’t been trying.
If you have these symptoms, it doesn’t necessarily mean that you have bowel cancer – they can also be symptoms of much less serious conditions. These include conditions such as irritable bowel syndrome. But if you have them, especially if they don’t go away and aren’t normal for you, contact a GP. Talk to a GP if you’re worried about blood in your poo too.
Sometimes, bowel cancer can cause a blockage (bowel obstruction). This can cause:
- sudden cramping pains in your tummy
- bloating
- constipation
- being sick
Seek immediate medical attention if you get these symptoms.
Diagnosis of bowel cancer
A GP will ask about your symptoms and your medical history. It may help to keep a diary to track your symptoms, which you can share with the GP. The GP will examine you by feeling around your tummy and inside your back passage (rectum) to check for any signs of lumps or swellings. For more information on this, see our FAQ: What happens during a rectal examination?
The GP may give you a blood test to see if you have other health conditions, such as anaemia. The blood test will check your general health too. They may ask you to provide a poo sample, to check for any hidden blood in your poo.
If the GP thinks your symptoms need further investigation, they’ll refer you to a specialist. This may be a medical consultant who specialises in bowel conditions (colorectal specialist). Your specialist may suggest some of the following tests.
- A colonoscopy. This will allow your doctor to look at the lining of your large bowel using a narrow, flexible, tube-like telescopic camera called a colonoscope. Your doctor can also use this to take a small sample of tissue (biopsy), which they’ll send to a lab to look for cancer cells.
- A sigmoidoscopy. This is similar to a colonoscopy, but just looks at the inside of your back passage and the lower part of your bowel. Your doctor may suggest it as an alternative to colonoscopy.
- A virtual colonoscopy. This uses a CT scan to create a three-dimensional image of the inside of your bowel. This option is offered in some areas if you aren’t well enough to have a colonoscopy. It’s also known as CT colonography.
If these tests find you have bowel cancer, you’ll need further tests to find the size and position of the cancer, and to check if it has spread. This is called staging and may include CT and MRI scans.
Screening for bowel cancer
If you’re registered with a GP surgery, they’ll invite you for bowel cancer screening every two years. When you’re invited for screening depends on where you live.
- In England, if you're between 60 and 74, you’ll be offered bowel cancer screening, and in some areas, from the age of 50.
- In Northern Ireland, if you’re between 60 and 74 you’ll be invited for screening.
- In Scotland, it’s offered between 50 and 74.
- In Wales it’s offered between the ages of 55 and 74.
You can also request a test if you're over 74. Screening is important because it may detect bowel cancer before you have symptoms. This is when treatment is likely to be more effective.
The screening kit, called the faecal immunochemical test (FIT), is sent to you to do at home. The test can detect small amounts of blood in your poo that you may not normally notice. It doesn't diagnose bowel cancer – but the results will show whether or not you need to have any further tests. If you have an abnormal screening result, you’ll be offered a colonoscopy.
While bowel cancer screening can help to detect cancer, it isn’t perfect and might not always pick it up. So it’s important to look out for symptoms, even if you’ve had a clear screening result.
Your GP surgery will have information about the bowel cancer screening programme in your area.
Looking for cancer cover that supports you every step of the way?
If you develop new conditions in the future, you can rest assured that our health insurance comes with full cancer cover as standard.
To get a quote or to make an enquiry, call us on 0800 600 500∧
Cancer awareness: Bowel cancer
Bowel cancer screening | Watch in 1:04 minutes
If you are aged 50-74 you will receive a bowel cancer screening kit every two years in the post. This animation explains how the kit is used and why it's important to detect bowel cancer early.
Treatment of bowel cancer
Your treatment for bowel cancer and care will be managed by a team of doctors and other cancer specialists. They’ll discuss what treatment for bowel cancer they recommend for you. This will depend on the size of your tumour (lump of cells), its position and if it has spread, as well as your general health and fitness.
If you find out you have bowel cancer early on, it may be possible to cure it. If you’re diagnosed later and the cancer has spread, the focus of treatment may be on prolonging your life and reducing your symptoms.
Surgery
If possible, your medical team will aim to remove the cancer with bowel surgery. This may be keyhole (laparoscopic) surgery, which means the surgeon will insert tiny instruments into several small cuts in your tummy, to perform the surgery. Or you may need to have open surgery, where your surgeon will make one large cut in your tummy.
Your surgeon will remove the affected part of your large bowel and, if possible, join the two open ends together. Sometimes they may form a stoma to give your bowel a chance to heal. This is where the end of your bowel is brought out to the surface of your tummy. A stoma bag is placed over the stoma to collect the waste from your bowel.
A stoma is usually temporary and can be reversed a few months later in another operation. But sometimes, if a lot of your bowel has been removed, a permanent stoma may be necessary. Most people won’t need this, but your surgeon will be able to let you know how likely it is for you. If you do need a stoma, a nurse will visit you after your operation to discuss with you how to care for your stoma.
Non-surgical treatments
You may have some of the following treatments as well as, or instead of, surgery.
- Chemotherapy – this uses medicines to kill cancer cells. You might have this before surgery to shrink the tumour (lump of cells) or after surgery to reduce the chance of the cancer coming back. If you’re not able to have surgery, you may have chemotherapy to help slow down the growth of cancer and reduce your symptoms.
- Radiotherapy – this uses radiation to destroy the cancer cells. You might have this if your cancer is in your rectum, alongside surgery and other treatments.
- Targeted cancer drugs – these are medicines that can seek out cancer cells and interfere with the way they grow. They’re sometimes used alongside chemotherapy for bowel cancer, especially if the cancer has spread to other parts of your body.
Prevention of bowel cancer
It’s not always possible to prevent bowel cancer. But there are certain changes you can make to your lifestyle to help keep your risk as low as possible.
- Keep to a healthy weight.
- Eat a healthy, balanced diet with plenty of fruit and vegetables, high-fibre foods, and low amounts of processed and red meat.
- Try to keep active by doing regular exercise.
- If you smoke, try to stop. Speak to your GP for advice and support on stopping smoking.
- Only drink alcohol in moderation – drink sensibly by keeping to recommended limits.
If you have a condition called Lynch syndrome, your doctor may recommend you take aspirin every day to help prevent bowel cancer. Ask your doctor for more information.
Screening for people at high risk of bowel cancer
If you’re at high risk of bowel cancer, you may need regular screening tests to check for any cancerous changes in your bowel. You’re at greater risk if, for example, you have a strong family history of bowel cancer or a particular health condition such as ulcerative colitis. If any polyps (growths of tissue) or areas of concern are spotted during your screening test, they may be removed to prevent cancer developing. Colon polyps can be removed with a procedure called a colonoscopy. Larger polyps may need to be removed by surgery.
If you think you may have an increased risk of getting bowel cancer, ask a GP about screening.
During a rectal examination, your doctor will put on some gloves and feel inside your back passage (rectum) with their finger. They’ll use lubricating gel. You may feel their finger moving around as they check for any lumps or abnormalities. This may feel uncomfortable but it shouldn’t hurt and only takes around 10 seconds. There’s no need to feel embarrassed – it’s an important medical test that your doctor has done many times before.
See our section on diagnosis of bowel cancer for more information.
Yes, bowel cancer is more likely if you have an inflammatory bowel disease such as Crohn’s disease or ulcerative colitis. You’ll be offered regular bowel cancer screening, from around 10 years after you first developed symptoms. How often you’re tested will depend on your risk – it may vary between once a year and once every five years.
See our section on causes of bowel cancer for more information.
Bowel cancer is most common in older people. Although you can develop bowel cancer at any age, it’s rare before 40. More than 40 out of 100 people diagnosed with bowel cancer in the UK are 75 or older.
See our section on causes of bowel cancer for more information.
Bowel cancer is likely caused by a mixture of different things. These include things like having a family history of bowel cancer or an inherited bowel condition such as Lynch syndrome that increases your risk. Your lifestyle can also affect your chances of getting bowel cancer. Things like your diet – if you don’t eat enough fibre and eat a lot of processed and red meats, it may increase your risk. It’s also important to do plenty of exercise and not smoke.
See our section on causes of bowel cancer for more information.
The main symptoms of bowel cancer include bleeding from your bottom or blood in your poo, and changes in your bowel habits. You might feel extremely tired and weak and pain or discomfort in your tummy or bottom that doesn’t go away.
See our section on symptoms of bowel cancer for more information.
Bowel surgery
There are lots of types of bowel surgery. Here we look at bowel resection...
Did our Bowel cancer information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Colorectal cancer. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 15 December 2021
- Lotfollahzadeh S, Kashyap S, Tsoris A, et al. Rectal cancer. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 3 December 2022
- What is bowel cancer? Cancer Research UK. www.cancerresearchuk.org, last reviewed 30 November 2021
- Colorectal cancer. BMJ Best Practice. bestpractice.bmj.com, last reviewed 9 December 2022
- NHS bowel cancer screening: Helping you decide. Public Health England. www.gov.uk, updated 28 July 2022
- Colorectal cancer. Patient. patient.info, last edited 20 October 2020
- Bowel cancer survival statistics. Cancer Research UK. www.cancerresearchuk.org, last reviewed 27 November 2019
- Risks and causes of bowel cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 3 December 2021
- Symptoms of bowel cancer. Bowel Cancer UK. www.bowelcanceruk.org.uk, reviewed July 2022
- Symptoms of bowel cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 3 December 2021
- Visiting your GP. Bowel Cancer UK. www.bowelcanceruk.org.uk, updated October 2022
- Colonoscopy for bowel cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 December 2021
- Flexible sigmoidoscopy. Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 December 2021
- CT colonography. Cancer Research UK. www.cancerresearchuk.org, last reviewed 7 December 2021
- Guidance. Bowel cancer screening: Programme overview. Public Health England. www.gov.uk, last updated 17 March 2021
- Bowel cancer screening. nidirect. www.nidirect.gov.uk, accessed 11 January 2023
- Scottish bowel screening programme statistics. Public Health Scotland. www.publichealthscotland.scot, published 2 February 2021
- Bowel screening Wales. Public Health Wales. phw.nhs.wales, accessed 11 January 2023
- Treatment. Bowel Cancer UK. www.bowelcanceruk.org.uk, accessed 11 January 2023
- Treating advanced bowel cancer. Bowel Cancer UK. www.bowelcanceruk.org.uk, updated November 2020
- Types of surgery for bowel cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 2 February 2022
- Targeted and immunotherapy drugs for advanced bowel cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 1 December 2021
- Screening for people at high risk of bowel cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 10 December 2021
- Bowel care. Management of lower bowel dysfunction, including digital rectal examination and digital removal of faeces. Royal College of Nursing. www.rcn.org.uk, published 11 September 2019
- Examination of your back passage. Cancer Research UK. www.cancerresearchuk.org, last reviewed 6 December 2021
- Colorectal cancer prevention: Colonoscopic surveillance in adults with ulcerative colitis, Crohn’s disease or adenomas. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 20 September 2021
- Crohn's disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2020
- What is cancer screening? Cancer Research UK. www.cancerresearchuk.org, last reviewed 10 November 2022
- Rachael Mayfield-Blake, Freelance Health Editor



