Back Surgery
Expert reviewer: Mr Radu Popa, Consultant Spinal Surgeon
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, May 2023
Next review due May 2026
Back surgery is a treatment for back pain, although most people don’t need surgery. Often, other treatments, such as painkillers, physiotherapy, injections, and psychological therapies can ease back pain. You’ll only have back surgery if these treatments don’t help and your doctor believes surgery will.
About back surgery
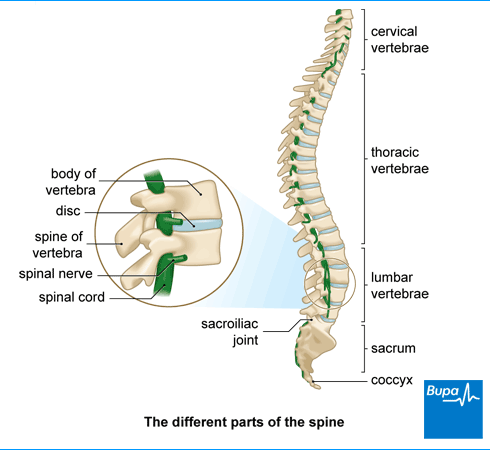
There are different types of back surgery and the operation you have will depend on the cause of your back pain. Some surgery helps to relieve back pain caused by wear and tear or osteoporosis. Other types can help if you have severe pain spreading down your leg (sciatica), caused by pressure on the nerves in your spine.
The most common types of back surgery are described below. Your spine surgeon will discuss which type of surgery is best for you, and explain what’s involved.
Lumbar decompression
Lumbar decompression (or spinal decompression) relieves pressure on trapped nerves that are causing pain in your back or legs. Decompression involves either discectomy, laminectomy or both.
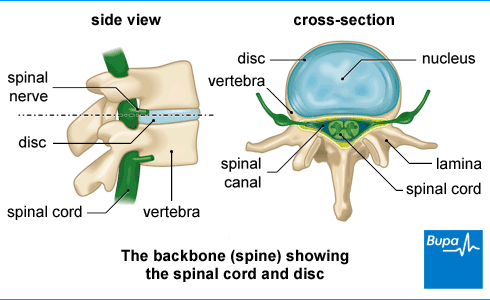
Discectomy is the partial or complete removal of a disc between your vertebrae (the bones in your spine). Your surgeon may recommend this if a disc is damaged and is pressing on surrounding nerves (known as a herniated or ‘slipped’ disc). This treatment isn’t the right choice if you have lower back pain. If your surgeon removes the whole disc, they may suggest replacing it with an artificial disc. Ask your surgeon to explain the different options to you.
Laminectomy involves removing a small piece of bone at the back of a vertebra, called the lamina. This opens up the centre of your spinal column to relieve pressure on the nerve. Your surgeon may suggest it for spinal stenosis – a condition which causes narrowing of your spinal canal.
Spinal fusionThis procedure joins two or more vertebrae together using bone grafts, screws and rods. It strengthens and stabilises your spine, and prevents painful movement. Your surgeon may recommend this:
- along with decompression surgery if one of your vertebrae slips out of place
- if your spine is unstable
- if the discs between the vertebrae in your spine are worn down (severe disc degeneration)
- for scoliosis, where your spine bends to one side
If you have lower back pain, your doctor won’t offer spinal fusion to you unless it’s part of a research trial.
Vertebroplasty and kyphoplasty
In vertebroplasty, your surgeon will inject glue-like bone cement into your vertebra to repair a compression fracture (collapsed vertebra), caused by osteoporosis or an injury. A similar procedure, called kyphoplasty, involves putting a special balloon in first, to lift the vertebra before the cement is injected.
Percutaneous coblation
In this procedure, your surgeon will use X-rays to guide them to the right spot in your back. They’ll then pass a heated probe through a needle to destroy a damaged disc.
Percutaneous endoscopic discectomy
In percutaneous endoscopic discectomy, a surgeon will remove tissue from a damaged disc with instruments that they’ll pass through a small cut or needle in your back.
Newer methods for back surgery, such as percutaneous coblation and percutaneous endoscopic discectomy, cause less damage to body tissues (less invasive) than standard techniques. This means you may recover quicker. Ask your surgeon if this is an option for you.
Preparation for back surgery
Before your operation
You'll meet your surgeon or someone from their team before the operation day. They’ll run through any other treatment options and ensure you understand the expected outcome of surgery. They'll discuss what will happen before, during, and after your procedure, and any pain or possible complications you might have. This is your opportunity to ask questions so you understand what will happen. If you decide to go ahead, you’ll be asked to sign a consent form.
Before your operation, it's worth preparing for your first days at home after surgery. You’ll usually be able to walk after your operation but may need some bed rest first. Ask family or friends if they can help you with things like washing, dressing, cleaning, and shopping. If you live alone, you may need someone to stay with you for the first few days. You’ll also need to be collected from hospital because you won’t be able to drive for a while.
If you’re having open surgery, you’ll probably have a general anaesthetic. You won’t be able to eat or drink before your surgery. Your anaesthetist or surgeon will give you advice on this. You can’t eat anything for about six hours before surgery, but you may be able to drink some water until two hours before. Follow your anaesthetist’s advice.
On the day
You may be given compression stockings to wear, to help prevent blood clots forming in the veins in your legs. And you may have an injection of an anticlotting medicine.
Your surgeon will check that you've signed the consent form and are still happy to go ahead.
Back surgery procedure
Decompression surgery and spinal fusion
You’ll have a general anaesthetic for these procedures, which means you’ll be asleep throughout. Your surgeon will take X-rays to find the affected area of your back, then make a cut into your back to reach your spine. The surgery will usually take between one and three hours, depending on exactly what’s being done. If you have a bigger operation, it can take as long as 10 to 12 hours.
In decompression surgery, your surgeon will remove sections of bone, ligaments, and disc to free up the nerves in your back. You may be able to have a smaller operation where only part of a vertebra is removed. If bone is removed, this is called a laminectomy. If only disc material is removed, it is called microdiscectomy surgery.
In spinal fusion, your surgeon inserts a bone graft (a small piece of bone) between two bones in your spine (vertebrae) to fuse them together. The graft may be from elsewhere in your body, from donated bone, or it may be artificial. You may have plates, screws and rods to keep your spine still while the bones fuse.
Vertebroplasty and kyphoplasty
These procedures are used to fix compression fractures, usually from osteoporosis, and to strengthen bone to prevent future fractures.
You may have a general or local anaesthetic. If you have a local anaesthetic, you’ll be awake during the operation, but your doctor will offer you a sedative medicine to relax you.
You’ll lie face down and your surgeon will put the needle into the affected area of your back (guided by X-rays). They’ll then inject cement into the broken bone. In kyphoplasty, your surgeon will put in a balloon temporarily to make space for the cement.
Aftercare for back surgery
After back surgery, you’ll go to a recovery room where a nurse will monitor you until you’re fully awake. You’ll have pain relief to help as the anaesthetic wears off.
You’ll probably have an intravenous (IV) drip in a vein in your arm. And you may have a catheter in your bladder, which will drain your pee (urine) into a bag. You'll have a dressing over your wound.
You’ll usually spend up to a few nights in hospital. You’ll need to spend some time resting in bed, but your hospital team will also encourage you to get up and walk around.
A nurse will give you advice about caring for your back and looking after your wound before you go home. A physiotherapist or your surgeon will give you some exercises to help you recover.
You’ll need to arrange for someone to drive you home. And if you live alone, ask a friend or relative to stay with you for the first few days.
Recovery for back surgery
Your recovery time from back surgery will depend on the type of surgery you've had. It also varies from person to person.
- After standard decompression surgery, you can usually expect to be pain free and able to exercise gently after 6 weeks. You should be back to most normal activities within 12 weeks.
- It can take several months for bone to grow after spinal fusion. You'll be told how to move in a way that keeps your spine aligned during this time. You’ll have physiotherapy and will be able to gradually increase your activities.
- For vertebroplasty and kyphoplasty, you should be back to usual activities straight away.
Getting over open surgery
Recovering from open back surgery takes longer than procedures that don’t involve making a cut in your back. Try to keep moving, and build up your activities gradually. If you feel tired, stop and rest. To start with, you’ll need help with practical tasks, such as cooking, cleaning and shopping.
Doing your physiotherapy exercises will help you get your strength and movement back and prevent stiffness. Your surgeon or physiotherapist may tell you not to do some activities and movements. For example, up to four weeks after surgery, don’t do any:
- heavy lifting
- twisting
- bending forward
- sitting or standing in one position for too long
Aim to build up the amount of exercise you do, starting with light exercise and gradually get back to normal.
Pain relief and looking after your wound
You may need pain relief in the first weeks after surgery. You can take over-the-counter painkillers , such as paracetamol or ibuprofen. Always read the patient information leaflet that comes with your medicine and if you have any questions, ask a pharmacist for advice.
You'll have a dressing over your wound when you come home. Wash carefully around this to keep it dry. Your stitches or staples will be removed about 10 days after surgery. After that, you can soak in a bath and shower as normal. When the wound has healed, you'll have a small scar.
Driving
You can usually drive about six weeks after surgery. But don’t drive if your painkillers make you drowsy, or before you can safely control your vehicle. Tell your insurance company about your operation and check your policy.
Getting back to work
How soon you can go back to work will depend on which type of surgery you had, and your job. Most people can return to work after about four to six weeks. If your job is strenuous or involves driving or heavy lifting, you may need up to 12 weeks off. Ask your surgeon or occupational health team.
Side-effects of back surgery
Side-effects of back surgery can include pain and some discomfort around the wound. You may feel the pain deep in your back, especially when you move around. How long it takes for the pain to go will depend on the type of back surgery you had, but it could take six weeks if you had decompression surgery, for example.
Physiotherapy services
Our evidence-based physiotherapy services are designed to address a wide range of musculoskeletal conditions, promote recovery, and enhance overall quality of life. Our physiotherapists are specialised in treating orthopaedic, rheumatological, musculoskeletal conditions and sports-related injury by using tools including education and advice, pain management strategies, exercise therapy and manual therapy techniques.
To book or to make an enquiry, call us on 0345 850 8399
Complications of back surgery
Complications specific to back surgery depend on the type of surgery but may include the following.
- A wound infection or an infection in the tissues around your spine. If this happens, you may need antibiotics.
- Bleeding – if you lost a lot of blood during surgery, you may need a transfusion.
- Damage to nerves, blood vessels or other tissues may occur. If the membrane covering your spine is damaged, the fluid surrounding your spinal cord (cerebrospinal fluid, CSF) can leak out. Your surgeon will mend this during surgery. A tear can cause headaches afterwards but these usually improve with time.
- A swelling of blood (haematoma) near your wound– this may need draining.
- After spinal fusion, the graft, rods and screws may break or move out of place. If this happens you’ll need another operation to repair it. You may also need a second operation if not enough bone forms.
- With vertebroplasty and kyphoplasty, the cement may leak or you may have a reaction to it.
- If your symptoms come back after surgery, or you have another slipped disc, for example, you may need further surgery
If you have any concerns about complications, talk to your surgeon about them. After you go home, contact the hospital if you have any concerns about ongoing symptoms and your recovery.
Alternatives to back surgery
Most people don’t need back surgery and can use non-surgical treatments to get better. Alternative treatments to back surgery include:
- exercise
- manual therapies, such as osteopathy and physiotherapy
- psychological therapies
- radiofrequency denervation
Yes, you can usually play sports again but only after your spine has recovered from back surgery. It takes most people about 12 weeks after surgery to get back to their normal activities (excluding contact sports). Start by taking short walks and after six weeks you could try swimming. This will put very little strain and pressure on your spine. Ask your surgeon for more advice.
There are different types of back surgery for different causes of back pain. Types of back surgery include discectomy, which is surgery for a ‘slipped’ disc. Other surgeries include laminectomy, which can relieve pressure on trapped nerves that cause pain in your back or legs. And spinal fusion, which can treat scoliosis, where your spine bends to one side.
For more information, see our section: About back surgery.
How long it takes to recover from back surgery will depend on the type of surgery you have. It also varies a lot from person to person. Recovering from open surgery takes longer than procedures that don’t involve making a cut in your back. For example, after decompression surgery, it can take about 6 to 12 weeks to recover. But for vertebroplasty and kyphoplasty, you should be back to usual activities almost straight away.
For more information, see our section: Recovery for back surgery.
It can be worth having back surgery if other non-surgical treatments haven’t helped you. It’s important to try other treatments first, such as exercise, physiotherapy , psychological therapies, and visiting a pain clinic. Here they may offer you radiofrequency denervation. These treatments might help and avoid the need to go through surgery. Ask your surgeon what’s best for you.
There are some things that you shouldn’t do after back surgery. For example, up to four weeks after surgery, don’t do any heavy lifting, twisting, or bending forward. It’s also best not to sit or stand in one position for too long.
For more information, see our section: Recovery for back surgery.
Lower back pain
Lower back pain is very common. It is often caused by straining muscles, tendons or ligaments in your back. Find out everything you need to know about lower back pain.
Osteoporosis
Physiotherapy
Did our Back Surgery information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Dydyk AM, Massa RN, Mesfin FB. Disc herniation. StatPearls Publishing.. www.ncbi.nlm.nih.gov, last update 18 January 2022
- Low back pain and sciatica in over 16s: assessment and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 11 December 2020
- Spinal stenosis. Patient. patient.info, last edited 21 September 2022
- Back pain. Versus Arthritis. www.versusarthritis.org, accessed 23 February 2023
- Osteoporotic spinal compression fractures. BMJ Best Practice. bestpractice.bmj.com, last reviewed 23 January 2023
- Spinal disc problems. Patient. patient.info, last edited 15 February 2022
- Estefan M, Munakomi S, Willhuber GOC. Laminectomy. StatPearls Publishing. www.ncbi.nlm.nih.gov, last update 9 August 2022
- Discogenic low back pain. BMJ Best Practice. bestpractice.bmj.com, last reviewed 23 January 2023
- Spinal fusion. American Academy of Orthopaedic Surgeons. orthoinfo.aaos.org, last reviewed 22 February 2022
- Patel A, Petrone B, Carter KR. Percutaneous vertebroplasty and kyphoplasty. StatPearls Publishing. www.ncbi.nlm.nih.gov, last update 12 September 2022
- Percutaneous coblation of the intervertebral disc for low back pain and sciatica. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 27 January 2016
- Percutaneous transforaminal endoscopic lumbar discectomy for sciatica. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 27 April 2016
- Consent and ethics: Adults. Royal College of Anaesthetists. www.rcoa.ac.uk, published 13 August 2019
- Preparing for low back surgery. American Academy of Orthopaedic Surgeons. orthoinfo.aaos.org, last reviewed April 2022
- Discectomy. Recovery tracker. Royal College of Surgeons of England. www.rcseng.ac.uk, accessed 24 February 2023
- Discectomy. Royal College of Surgeons of England. www.rcseng.ac.uk, accessed 24 February 2023
- Lumbar discectomy. Medscape. emedicine.medscape.com, updated 24 September 2019
- Debono B, Wainwright TW, Wang MY, et al. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced recovery after surgery (ERAS®) society recommendations. NASS 2021; 21(5):729–52. doi: https://doi.org/10.1016/j.spinee.2021.01.001
- Venous thromboembolism in over 16s: Reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 13 August 2019
- Lumbar discectomy technique. Medscape. emedicine.medscape.com, updated 24 September 2019
- Dowling TJ, Dowling TJ, Munakomi S. Microdiscectomy. www.ncbi.nlm.nih.gov, last update 25 February 2022
- Osteoporosis and spinal fractures. American Academy of Orthopaedic Surgeons. orthoinfo.aaos.org, last reviewed November 2021
- Anaesthesia explained. Royal College of Anaesthetists. www.rcoa.ac.uk, published 1 March 2021
- Discectomy. What to expect after the operation. Royal College of Surgeons of England. www.rcseng.ac.uk, accessed 24 February 2023
- Spinal stenosis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 23 January 2023
- Spinal instability and spinal fusion surgery. Medscape. emedicine.medscape.com, updated 15 March 2022
- Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for treating osteoporotic vertebral compression fractures. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 24 April 2013
- Back pain – low (without radiculopathy). NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised November 2022
- Managing your back pain. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 19 July 2022