Ectopic pregnancy
- Mr Olayemi Kuponiyi, Consultant Obstetrician & Gynaecologist
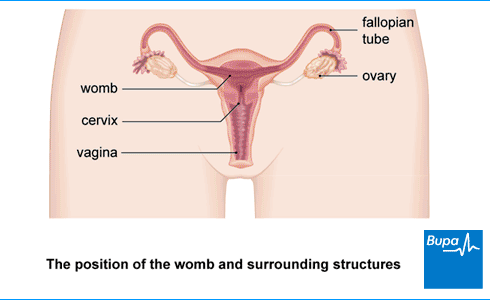
An ectopic pregnancy is when a fertilised egg implants outside the lining of your womb (uterus). Signs of ectopic pregnancy may include pain in your pelvis or tummy, and unusual bleeding from your vagina. Unfortunately, the fertilised egg can’t survive, and it won’t be possible to save the pregnancy.
About ectopic pregnancy
In a healthy pregnancy, your ovary releases an egg and this is fertilised by sperm in one of your fallopian tubes. The fertilised egg travels to your womb where it implants in the lining and grows into a baby. But in around 1 in every 100 pregnancies, the fertilised egg implants in the wrong place. This is nearly always in one of your fallopian tubes. When the fertilised egg implants in a fallopian tube, it can’t grow into a baby.
If you have an ectopic pregnancy, it may end by itself or the egg may keep growing. If the egg keeps growing, it may eventually split (rupture) the fallopian tube. This can cause life-threatening internal bleeding. So, if you have an ectopic pregnancy, you may need immediate treatment to prevent complications like this.
Causes of ectopic pregnancy
Doctors don’t always know why an ectopic pregnancy happens. But some things may make you more likely to have one. These include:
- pelvic inflammatory disease or sexually transmitted infections – these can damage your fallopian tubes, which makes it harder for the egg to pass through them
- a previous ectopic pregnancy
- problems with infertility
- if you had a sterilisation operation – if the surgery doesn’t work and you get pregnant, it’s possible you could have an ectopic pregnancy
- smoking
- being over 35
- if you’ve had in-vitro fertilisation (IVF)
If you use contraception, it will lower your chances of having an ectopic pregnancy because you’re much less likely to get pregnant. But if you do get pregnant while using certain types of contraception, you may be more likely to have an ectopic pregnancy. These contraception methods include:
- intrauterine device (IUD)
- intrauterine system (IUS)
- the progestogen-only pill (POP)
If you’re using one of these forms of contraception and you think you may be pregnant, see your GP as soon as possible. If you do have an ectopic pregnancy, it’s easier to treat if it‘s diagnosed early on – and your chances of complications will be lower.
It isn’t possible to prevent an ectopic pregnancy, but you may be able to reduce your risk by:
- giving up smoking
- protecting yourself against sexually transmitted infections (STIs), which can damage your fallopian tubes
Symptoms of ectopic pregnancy
Ectopic pregnancy symptoms usually appear about six to eight weeks after your last period.
Symptoms or signs of ectopic pregnancy include:
- not having periods
- pelvic or tummy pain – the pain may develop gradually or come on suddenly
- bleeding from your vagina, which may be different from your normal period – it may be lighter, heavier or darker, and may contain clots
- pain in the tip of your shoulder – this is caused by bleeding into your tummy, which irritates nerves that run to your shoulder
- feeling dizzy or fainting
- diarrhoea and being sick
- needing to poo constantly and feeling uncomfortable when you poo
Not everyone with an ectopic pregnancy gets these symptoms. You may have no symptoms at all or you may have only one or two symptoms. Sometimes, an ectopic pregnancy is suspected when you have an early scan, even though you feel well. Everyone is different.
Ectopic pregnancy symptoms are similar to the symptoms of a miscarriage so it can be difficult to tell the difference at first. In a miscarriage, vaginal bleeding is usually the main symptom, with some pain later on. In an ectopic pregnancy, the pain usually comes first – there may be some vaginal bleeding, but not always.
If you’ve missed a period or could be pregnant and have any of the above symptoms, contact your doctor immediately.
Diagnosis of ectopic pregnancy
Your GP will ask about your symptoms and medical history. They’ll also examine you and offer you a pregnancy test. If your pregnancy test is negative, it’s unlikely that your symptoms are being caused by an ectopic pregnancy.
If your pregnancy test is positive or your symptoms strongly suggest you have an ectopic pregnancy, your GP may refer you to a hospital specialist. You may go to a clinic called an early pregnancy assessment unit (EPAU). If you have severe symptoms of an ectopic pregnancy, your GP will call an ambulance to get you straight to hospital as an emergency.
At the clinic or hospital, you may have some further tests.
- A transvaginal ultrasound scan. Sound waves from a probe inside your vagina help your doctor see where the pregnancy is. You may also have a tummy ultrasound. It can sometimes be hard to spot an ectopic pregnancy with an ultrasound scan so you may need to have the scan again.
- A blood test. This will measure a pregnancy hormone called human chorionic gonadotrophin (hCG). Your doctor may repeat this test after two days to see how much the level of hCG goes up. It goes up less in an ectopic pregnancy than in a normal pregnancy that’s growing inside the womb.
- A laparoscopy (keyhole surgery). You may need this when it’s still unclear whether or not you have an ectopic pregnancy, especially if you’re unwell. Your surgeon will use a narrow, tube-like, telescopic camera (called a laparoscope) to look at your fallopian tubes, ovaries and tummy. They put the laparoscope into your tummy through a small cut. You will usually be given a general anaesthetic for a laparoscopy, so you’ll be asleep during the procedure.
Treatment of ectopic pregnancy
An ectopic pregnancy can’t develop normally so all treatments lead to the end of the ectopic pregnancy.
Here we describe the treatment options for an ectopic pregnancy in the fallopian tubes – the most common kind of ectopic pregnancy. If you have an ectopic pregnancy somewhere else, your doctor will talk to you about the possible treatment options.
Your ectopic pregnancy treatment will depend on:
- how severe your symptoms are
- how advanced your ectopic pregnancy is
- whether or not your fallopian tube has split open
Your doctor will also ask if you plan to get pregnant in the future.
For more information, see our section on help and support.
Watchful waiting (expectant management)
You may not need any treatment for an ectopic pregnancy because sometimes the pregnancy ends by itself.
Before your doctor decides if this is a safe option for you, they’ll check that:
- the mass in your fallopian tube is smaller than three-and-a-half centimetres
- you have little or no pain and your doctor isn’t worried about anything else to do with your health
- your blood test shows the level of hCG is low and falling
- you’re happy to agree to being monitored by the hospital
Your doctor will ask you to have regular blood tests for hCG until it can’t be detected anymore. You don’t have to stay in hospital, but you should go back if you have any more symptoms –for example, bleeding or pain.
Expectant management is successful for around 8 out of every 10 people who have it. If it doesn’t work for you, you can go on to have medical treatment or ectopic pregnancy surgery if necessary.
Medicines
Medical treatment for ectopic pregnancy involves having one or more injections of a medicine called methotrexate. This will stop the embryo cells growing, and the pregnancy will gradually be absorbed by your body. Methotrexate treatment is only suitable if your ectopic pregnancy is still in the early stages.
After your injection, you’ll need to return for further monitoring of your hCG levels. Depending on the results, you may need another dose of methotrexate. You’ll have blood tests until hCG is no longer found in your blood.
Treatment with methotrexate can cause some side-effects. It often causes tummy pain for two or three days after the injection. It may also cause sickness and diarrhoea.
It’s important not to get pregnant again for at least three months after you have a methotrexate injection. If you get pregnant during this time, methotrexate may harm your developing baby.
Some people can’t be treated with methotrexate because of their general health. If you can’t have methotrexate or if the medicine doesn’t work, your doctor will suggest you have surgery.
Surgery
You may need surgery to take away your fallopian tube (or part of it) and the ectopic pregnancy if:
- medicines haven’t worked or you’re unable to keep going back for follow-up tests after medical treatment
- your ectopic pregnancy is larger than 3.5 centimetres (1.4 inches) across
- you have severe pain
- you’re very unwell because your fallopian tube has ruptured, and you have internal bleeding – this is a medical emergency
You’ll have ectopic pregnancy surgery under general anaesthesia. Usually, you’ll have keyhole surgery using a laparoscope. Your surgeon will put the laparoscope into your body through a small cut or cuts in your tummy. But sometimes they’ll need to make a larger cut to see the affected area directly. This is called open surgery or a laparotomy.
A salpingectomy is surgery that takes away your whole affected fallopian tube. You’ll usually have a salpingectomy if:
- you’ve had a previous ectopic pregnancy in the same fallopian tube
- you don’t plan to get pregnant in the future
- your fallopian tubes are badly damaged
A salpingostomy will take away the ectopic pregnancy but leave your fallopian tube in place. This gives your fallopian tube a chance to work normally in future. You may have a salpingostomy if:
- you want to get pregnant in the future
- you have other reasons for low fertility
If you have a salpingostomy, you’ll need to have follow-up tests to check your hCG levels. You may need to have the fallopian tube removed in the future.
Help and support
Having an ectopic pregnancy can affect you emotionally as well as physically. Everyone is different, but you may feel sadness and a sense of loss after an ectopic pregnancy. It may have been a worrying or frightening experience, especially if you needed emergency treatment. You may find it upsetting to go back to the hospital for repeated blood tests. You may also be worried about whether you’ll be able to get pregnant again in the future.
If you can, try to talk to someone about how you’re feeling. This may be a friend or relative or perhaps a bereavement counsellor. Ask your doctor for information about the support available to you.
You may find it helpful to look for information, advice and support online. Our section on other helpful websites lists some organisations that can help. These have helplines and support forums where you can talk to others about your experiences to help you recover.
Future pregnancies
Your periods may start again after four to six weeks. Ask your doctor when it’s safe to start having sex again. This may depend on which type of treatment you had, if any. If you had methotrexate injections, you’ll need to use reliable contraception for at least three months – our section on the treatment of ectopic pregnancy explains why.
If you’ve had an ectopic pregnancy, your chance of having a normal pregnancy afterwards is good. Even if you had your fallopian tube removed to treat the ectopic pregnancy, your chance of getting pregnant may only be slightly reduced.
But, if you’ve had one ectopic pregnancy, you’re more likely to have another one. Up to 1 in 5 women will have a second ectopic pregnancy. So, if you get pregnant again, it’s important to see your GP as soon as you find out. You’ll need to have an ultrasound scan six to seven weeks into your pregnancy to check the embryo is developing in your womb.
Ectopic pregnancies usually happen in the fallopian tubes and can’t develop normally. In an ectopic pregnancy, the fertilised egg is growing outside the womb and can’t survive.
For more information, see our section: About ectopic pregnancy.
Not everyone has signs of an ectopic pregnancy. But symptoms of ectopic pregnancy may include a missed period, some pelvic or tummy pain and bleeding from your vagina.
For more information, see our section on symptoms of ectopic pregnancy.
Symptoms of an ectopic pregnancy usually first appear around six to eight weeks after your last period. An ectopic pregnancy may be picked up in an early scan even if you feel well.
For more information, see our section on diagnosis of ectopic pregnancy section.
There isn’t one main cause of ectopic pregnancy and sometimes doctors don’t know why it happens. But some things may make you more likely to have one. These include if you’ve had pelvic inflammatory disease or sexually transmitted infections. These can damage your fallopian tubes, which makes it harder for the egg to pass through them. Smoking or being over 35 can also increase your risk of ectopic pregnancy
For more information, see our section on causes of ectopic pregnancy.
An ectopic pregnancy usually lasts about 6 to 16 weeks. The longer it lasts, the more bleeding and potential complications you may get. If you’ve missed a period or think you could be pregnant and have any ectopic pregnancy symptoms, contact your doctor.
Miscarriage
Pelvic inflammatory disease
Pelvic inflammatory disease (PID) is inflammation of the upper part of a woman’s reproductive organs.
Did our Ectopic pregnancy information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Ectopic pregnancy. BMJ Best Practice. bestpractice.bmj.com, last reviewed 14 August 2024
- Ectopic pregnancy. MSD Manuals. msdmanuals.com, reviewed/revised October 2023
- Ectopic pregnancy. Medscape. emedicine.medscape.com, updated 9 August 2024
- Mummert T, Gnugnoli DM. Ectopic pregnancy. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 8 August 2023
- Ectopic pregnancy. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2023
- Ectopic pregnancy. Patient. patient.info, updated 24 May 2021
- Baker M, dela Cruz J. Ectopic pregnancy, ultrasound. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 16 January 2023
- Gynecologic laparoscopy. Medscape. emedicine.medscape.com, updated 17 March 2023
- Ectopic pregnancy and miscarriage: Diagnosis and initial management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 23 August 2023
- Surgical management of ectopic pregnancy. Medscape. emedicine.medscape.com, updated 10 September 2024
- Salpingostomy and salpingectomy. Medscape. emedicine.medscape.com, updated 15 November 2022
- Ectopic pregnancy. Miscarriage Association. www.miscarriageassociation.org.uk, accessed 24 September 2024
- Ectopic pregnancy FAQs. Ectopic Pregnancy Foundation. www.ectopicpregnancy.co.uk, accessed 24 September 2024
- Rachael Mayfield-Blake, Freelance Health Editor



