Hysterectomy
- Dr Madhavi Vellayan, Consultant Gynaecologist
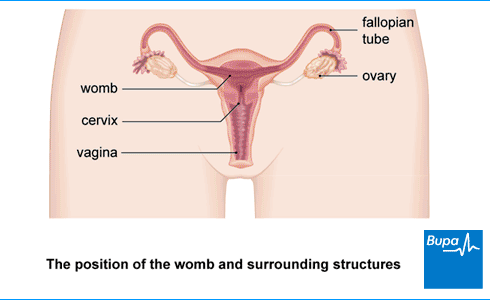
A hysterectomy is an operation to remove your womb (uterus). It can be a treatment option for several different medical conditions. After a hysterectomy, you’ll no longer have periods and you won’t be able to get pregnant.
About hysterectomy
You might have a hysterectomy for the following health conditions.
- Painful, heavy or frequent periods.
- Fibroids – non-cancerous growths of muscle and fibrous tissue in your womb.
- Endometriosis – when the cells that usually line your womb also grow outside it.
- Adenomyosis – when cells that usually line your womb grow into the womb muscle instead.
- Prolapse of your womb – when your womb has dropped down from its normal position.
- Cancer of the womb, cervix or ovaries, vagina or fallopian tubes.
For most of these conditions, you’ll usually try other treatments first. But if they don't work, or if your symptoms are severe, your GP may refer you to a gynaecologist for further investigation and treatment. A gynaecologist is a doctor who specialises in women’s reproductive health.
Your gynaecologist will talk to you about your treatment options, including any possible alternatives and the benefits and risks of having a hysterectomy. They’ll explain exactly what will happen before, during and after the procedure.
Take your time in making a decision about having a hysterectomy. It’s a major operation. For some people, an end to their symptoms following a hysterectomy is a huge relief. But others find it hard to come to terms with having their womb removed. Be sure to ask your doctor if you have any questions. You’ll be asked to sign a consent form before the procedure, so it’s important that you feel fully informed.
Types of hysterectomy surgery
There are three main ways to do a hysterectomy.
- Abdominal hysterectomy. Your surgeon makes a cut in your abdomen (tummy) to reach your womb.
- Vaginal hysterectomy. The surgeon will carry out the operation through your vagina.
- Laparoscopic hysterectomy (‘keyhole surgery’). Your surgeon does the surgery using a camera and instruments inserted through small cuts in your abdomen.
There are also different types of hysterectomy.
- In a total hysterectomy, both your womb and cervix are removed.
- In a subtotal hysterectomy your womb is removed but your cervix is left in place.
- A radical hysterectomy involves removing surrounding tissues in addition to your womb and cervix.
- An oophorectomy or salpingo-oophorectomy involves removing one or both ovaries and fallopian tubes. You may have this at the same time as your hysterectomy.
Whichever type you have, you won’t have periods and you’ll no longer be able to get pregnant after a hysterectomy.
If you have your ovaries removed as well as your womb, you will go through the menopause straight after the operation. This is called a surgical menopause. If you have a hysterectomy without having your ovaries removed, you may still go through the menopause earlier than usual. Your doctor will talk to you about this and the treatments available to help with menopause symptoms.
If your cervix is removed as part of your hysterectomy, you’ll no longer need cervical screening (‘smear’) tests after the operation. If you have a hysterectomy that leaves your cervix in place, you should carry on having cervical screening tests.
The type of hysterectomy you’re offered and how it’s done will depend on a number of factors. These include why you’re having it, how severe the problem is and whether you have any other health conditions. Talk to your doctor about your options, and what would be best for you in your particular circumstances.
Preparing for a hysterectomy
Before the operation
Your doctor will give you information about how to prepare for your operation. For example, if you smoke, they will ask you to stop. Smoking increases your risk of complications during and after your surgery. It can also slow your recovery.
You may need to have some tests, such as blood tests and an electrocardiogram (ECG) before your operation. This is to make sure that you’re well enough for the operation to go ahead as planned.
How long you need to stay in hospital depends on what type of hysterectomy you have, and how the operation is done. It’s usually between one and four days, but it may be longer if you’re having a hysterectomy to remove cancer. Your surgeon can advise you before the procedure. Make sure you arrange for someone to drive you home after your operation..
On the day
You’ll usually need to stop eating and drinking around six hours before your operation. You may be able to continue drinking water up to two hours beforehand. Make sure you follow any instructions your hospital gives you.
At the hospital, you’ll be asked to wear compression stockings to help prevent blood clots forming in the veins in your legs. You may have an injection of an anti-clotting medicine too.
You’ll meet your surgeon before the procedure. They will check whether you’re happy to go ahead before asking you to sign a consent form.
Hysterectomy procedure
If you’re having an abdominal or a laparoscopic hysterectomy, you’ll usually have it under general anaesthesia. This means you’ll be asleep during the operation. For a vaginal hysterectomy, you may be able to have a spinal anaesthetic or epidural rather than a general anaesthetic. With a spinal anaesthetic or epidural, you’ll be awake but you’ll feel no pain from the waist down.
How the procedure is carried out depends on the type of hysterectomy you are having.
Abdominal hysterectomy
Your surgeon will make a cut across your lower abdomen (tummy). The cut is usually along your bikini line. Sometimes your surgeon will make the cut from your belly button down to your bikini line instead. Your surgeon then removes your womb and any other parts – such as your cervix, ovaries and fallopian tubes, through the cut.
At the end of the operation, they’ll close your wound with stitches, staples, clips or tape. Your doctor may leave a thin tube called a drain inside your wound. It helps to drain away any blood or fluid that builds up. Your nurse will take this out while you’re still in hospital.
Vaginal hysterectomy
In this method, your surgeon uses special instruments inserted into your vagina to carry out the operation. They’ll make a cut in the top of your vagina, and take out your cervix and womb through the cut. They will then close the cut in your vagina using stitches.
Your doctor may also use laparoscopic instruments inserted through small cuts in your abdomen to help carry out the operation. This is called a laparoscopic-assisted vaginal hysterectomy.
Laparoscopic hysterectomy
Laparoscopy is sometimes called ‘keyhole surgery’. In this procedure, your surgeon makes one or more small cuts in your lower abdomen. They’ll insert a tube into one of the cuts and gently inflate your abdomen using carbon dioxide gas. This allows your surgeon to see inside your abdomen more clearly. Your surgeon will then insert special surgical instruments with a tiny camera to remove your womb and cervix.
Aftercare for hysterectomy
In hospital
You’ll be in a recovery room once you wake up after your operation. You’ll need to rest until the effects of your anaesthetic have worn off. You’ll usually feel sleepy after a general anaesthetic and you might find it difficult to think clearly. This should pass within 24 hours. You might have some discomfort as the anaesthetic wears off but you'll be offered pain relief.
You will have a catheter in for about 24 hours after your operation. This drains urine through a tube and into a bag. Your nurse will remove it once you’re able to get up out of bed and move around. You may also have a drip to give you fluids and pain medication. After a vaginal hysterectomy, you may have a gauze pack inside your vagina to control bleeding for the first 24 hours. A nurse will remove this before you go home.
You’ll be able to start eating and drinking as soon as you feel ready. Eating and drinking can help you get back to normal and feel ready to go home.
Going home
Your healthcare team will monitor you and tell you when you can go home. This might be within the first 24 hours for a vaginal or laparoscopic hysterectomy, but it can be after two or three days. It’s likely to be between two and four days following an abdominal hysterectomy. You won’t be able to drive straightaway, so you’ll need someone to take you home.
Caring for your wounds
Before you go home, your nurse will advise you about caring for your wounds and may arrange a date for a follow-up appointment.
You should be able to have a shower or bath and remove any dressings the day after your operation. But make sure you dry your healing wounds by patting them afterwards.
If you’ve had a vaginal hysterectomy, you won’t have any wounds on the outside of your body. Stitches inside your vagina will be dissolvable, but you may notice them coming out on their own after a few days or weeks. This is normal.
Often, any stitches you have will dissolve on their own and you won’t need to have them removed. But sometimes with an abdominal or laparoscopic hysterectomy, you may have stitches or staples that need to be removed. This can usually be done by the practice nurse at your GP surgery around five to seven days after your operation.
Recovery from hysterectomy
It takes between four and eight weeks to recover after a hysterectomy. But this is different for everyone. Although you need to rest, it will help with your recovery to start doing some gentle exercise and getting back to your normal activities. Build up your activity slowly and gradually. Don’t lift anything heavy or do any strenuous activity for at least three to four weeks after having a hysterectomy.
Having sex
You can start having sex around six weeks after your operation. This is how long it takes for scars to heal both inside and outside your body. You won’t need to use contraception to prevent pregnancy after a hysterectomy. But you may still need to use condoms to protect against sexually transmitted infections (STIs).
Pelvic floor exercises
It’s important to do pelvic floor exercises as part of your recovery, to strengthen these muscles. Your pelvic floor muscles help to hold your abdominal organs in the right place and keep your bladder and bowel closed. You may see a physiotherapist before you’re discharged from hospital, who will show you how to do these.
Going back to work
When you go back to work will depend on the type of job you do, how physical it is and how well you feel. It might be two to three weeks after surgery if you’re feeling well and there are no complications from your surgery. But it can take up to six to eight weeks for some people, especially if your job is more physical. You’ll usually recover faster following a vaginal or laparoscopic hysterectomy than an abdominal hysterectomy.
Driving
If you’ve had a vaginal or laparoscopic hysterectomy, it can take two to four weeks before you feel comfortable and safe enough to drive. If you’ve had an abdominal hysterectomy, this may take longer. You should check with your motor insurance provider in case they have specific conditions for driving after surgery.
Side-effects of a hysterectomy
Hysterectomy side-effects can include the following.
- Pain and discomfort in your lower abdomen for a few days after your operation. Your nurse will provide you with some painkillers to manage this.
- Pain in your shoulder following a laparoscopic hysterectomy. It’s caused by the gas used to inflate your tummy irritating a nerve. You can take painkillers to manage this.
- Trapped wind. This is caused by your bowel temporarily slowing down and can cause some discomfort. Walking around as much as you can will help with this.
- Light bleeding or spotting from your vagina for up to six weeks after your operation. Wear a sanitary pad, rather than using a tampon, until any bleeding stops.
Complications of a hysterectomy
Complications are problems that can occur during or after the operation. Some of the possible complications after a hysterectomy are as follows.
- Heavy bleeding (more than would normally be expected after hysterectomy). This is more common after abdominal hysterectomy.
- Infection of your wound. The skin around your scars may become very red and sore.
- Vaginal infection following vaginal hysterectomy. You may have a fever, foul-smelling discharge from your vagina and pain in your pelvis.
- A urine infection. You may need to pee urgently and more often, have pain or discomfort when you’re peeing and smelly or cloudy pee.
- Damage to blood vessels or organs in your abdomen, including your bowel and bladder. This is more common after vaginal and laparoscopic hysterectomy. It can cause loss of sensation in your bladder, needing to pee more often and constipation. If you have severe or worsening pain, vomiting and a fever, you should seek medical attention.
- Deep vein thrombosis (DVT) – a blood clot in a vein in your lower leg. This may cause your leg to become red, swollen and painful. It can be dangerous if it travels to your lungs (pulmonary embolism).
Contact the hospital where you had your hysterectomy if you develop any problems. You should seek urgent medical attention if you have severe pain, or signs of an infection or DVT.
Sepsis (adults)
Sepsis is a life-threatening complication that can develop if you get an infection. Sepsis is a medical emergency. Call 999 or go to A&E immediately if you have any of the following symptoms.
- Slurred speech, confusion, difficulty making sense.
- Extreme shivering or muscle pain.
- Passing no pee (urine) during a day.
- Severe difficulty breathing, feeling breathless, or breathing very fast.
- It feels like you’re going to die.
- Skin changes, such as your skin looking blue, pale or blotchy, or a rash that does not fade when you roll a glass over it.
Alternatives to hysterectomy
Depending on why you have been offered hysterectomy, there may be alternative treatments you can try. For conditions like fibroids and
- Myomectomy. This is surgery to remove fibroids. It doesn’t remove your womb, so it won’t affect your ability to get pregnant.
- Endometrial ablation. This is a procedure to treat heavy periods. It destroys the lining of your womb, but avoids a major operation like hysterectomy to remove your womb.
- Uterine artery embolisation. This is a procedure to treat fibroids. It involves an injection to cut off the blood supply to the fibroids. This destroys them or stops them growing.
If you have cancer of your womb, hysterectomy is usually the only possible option to cure the cancer.
Whatever your situation, talk to your doctor about the treatment choices available to you.
Worried about your gynaecological health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0370 218 8122
It’s best to wait six weeks after your surgery before you start having sex. This allows your body to heal properly. You can’t get pregnant after a hysterectomy, so you don’t need to use contraception. But remember that you may still need to use a condom to protect against sexually transmitted infections (STIs). Read our Recovery section to find out more.
If you have your ovaries taken out as well as your womb, you will go through the menopause straightaway. If you have a hysterectomy without having your ovaries taken out, you may still go through the menopause earlier than normal. See our section on Types of hysterectomy surgery for more information.
You won’t have periods any more after having a hysterectomy, and you won’t be able to get pregnant. A hysterectomy involves removing your womb (uterus). See our Types section to find out more.
For most people, it takes between four and eight weeks to recover from a hysterectomy. This is different for everyone. It can depend on the type of operation you are having and your general health. See our Recovery section for more information.
If you’ve had a total hysterectomy and had your cervix removed, you’ll no longer need to have cervical smear tests. If you’ve had a subtotal hysterectomy, which leaves your cervix in place, you should carry on having the tests. Read our Types section for more information.
Menopause
Hormone replacement therapy (HRT)
Endometriosis
Fibroids
Did our Hysterectomy information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Hysterectomy. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, accessed 26 September 2022
- Carugno J, Fatehi M. Abdominal hysterectomy. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 5 December 2021
- Pillarisetty LS, Mahdy H. Vaginal hysterectomy. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 8 May 2022
- Heavy menstrual bleeding: assessment and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 24 May 2021
- Endometrial ablation. Medscape. emedicine.medscape.com, updated 16 April 2021
- Endometriosis: diagnosis and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 6 September 2017
- Uterine artery embolisation for treating adenomyosis. National Institute for Health and Care Excellence. www.nice.org.uk, published 16 December 2013
- Urinary incontinence and pelvic organ prolapse in women: management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 24 June 2019
- Menorrhagia. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised December 2018
- Obtaining valid consent. Clinical Governance Advice No. 6. Royal College of Obstetricians and Gynaecologists. www.rcog.org.uk, published January 2015
- Hysterectomy. Medscape. emedicine.medscape.com, updated 3 May 2021
- Risks and side effects of hysterectomy. Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 4 November 2020
- Ceasing and deferring women from the NHS cervical screening programme. Public Health England. www.gov.uk, updated 20 September 2019
- Anaesthesia explained. Royal College of Anaesthetists. www.rcoa.ac.uk, published January 2021
- Having a hysterectomy. Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 8 March 2021
- Personal communication, Dr Madhavi Vellayan, Consultant Gynaecologist, 20 October 2022
- You and your anaesthetic. Royal College of Anaesthetists. www.rcoa.ac.uk, published February 2020
- Your spinal anaesthetic. Royal College of Anaesthetists. www.rcoa.ac.uk, published February 2020
- Deep vein thrombosis (DVT) prevention. MSD Manual. www.msdmanuals.com, last full review/revision September 2022
- Surgical wounds – principles of wound management. Oxford handbook of adult nursing. Oxford Academic. academic.oup.com, published online June 2018
- Caring for someone recovering from a general anaesthetic or sedation. Royal College of Anaesthetists. www.rcoa.ac.uk, published November 2021
- Abdominal hysterectomy – recovering well. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, reviewed 22 October 2015
- Laparoscopic hysterectomy – recovering well. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, last reviewed 2015
- Vaginal hysterectomy – recovering well. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, last reviewed 2015
- Hysterectomy. Macmillan Cancer Support. www.macmillan.org.uk, last reviewed 1 April 2021
- Kaloo P, Armstrong S, Kaloo C, et al. Interventions to reduce shoulder pain following gynaecological laparoscopic procedures. Cochrane Database of Systematic Reviews 2019, Issue 1. Art. No.: CD011101. DOI: 10.1002/14651858.CD011101.pub2
- Nagle SM, Stevens KA, Wilbraham SC. Wound assessment. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 4 July 2022
- Urinary tract infection (lower) – women. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised June 2021
- Deep vein thrombosis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2022
- Florence AM, Fatehi M. Leiomyoma. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 18 July 2022
- Endometrial cancer. BMJ Best Practice. bestpractice.bmj.com, last reviewed 28 August 2022
- Pippa Coulter, Freelance Health Editor



