Polycystic ovary syndrome
- Dr Madhavi Vellayan, Consultant Gynaecologist
Polycystic ovary syndrome (PCOS) is a common condition affecting your ovaries. It can cause irregular periods, unwanted facial and body hair, and acne. It can also make it more difficult for you to get pregnant. PCOS treatment can help to ease symptoms, prevent complications, and improve your chances of pregnancy.
PCOS treatment can help to ease symptoms, prevent complications, and improve your chances of pregnancy.
About polycystic ovary syndrome
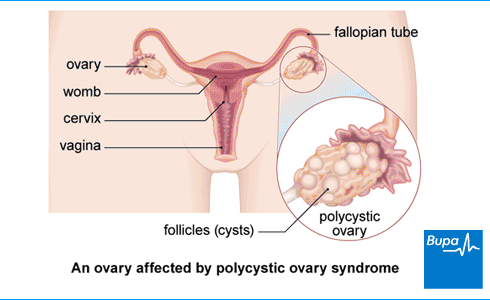
Polycystic ovary syndrome (PCOS) affects up to 1 in 10 women. There are two ovaries that are part of a woman’s reproductive system. They store and release eggs, and produce sex hormones. About once a month, one ovary should release an egg, ready to be fertilised.
Eggs develop in small fluid-filled swellings, called follicles. Each month, more than one follicle starts to develop. But usually only one becomes a fully mature egg. In polycystic ovary syndrome (PCOS), 12 or more follicles start to grow. But often none develop into an egg that can be fertilised and you don’t have a period that month. The follicles range in size from 2mm to 9mm, and stay on your ovaries containing undeveloped eggs. Despite the name, it’s actually follicles that are on your ovaries, not cysts.
You can have lots of follicles on your ovary without having PCOS. You can also have PCOS without having any follicles on your ovaries.
Causes of polycystic ovary syndrome
Doctors don’t know exactly why women get polycystic ovary syndrome (PCOS). But there are likely to be a few causes working together.
PCOS can run in families. So you may have a higher risk of developing PCOS if your mother or sister has the condition. Researchers have found several genes that are linked to an increased risk of PCOS. But it’s complicated because these genes are also common in women who don’t have PCOS. So they haven’t yet found genes that definitely cause the condition.
Many different hormones work together during a woman’s reproductive and menstrual cycle. In PCOS, some of these are out of balance. Your body may produce too much luteinising hormone (LH). This hormone helps to control the menstrual cycle.
Women naturally produce small amounts of the sex hormone testosterone. But in PCOS, your body may be making too much. This may be because your cells are resistant to insulin. This hormone helps your body to control the level of sugar in your blood. If your cells are resistant to insulin, your body makes more than it should. The extra insulin causes your ovaries to make too much testosterone.
All these hormone changes can stop your ovaries from releasing an egg each month.
Symptoms of polycystic ovary syndrome
PCOS symptoms usually start around puberty, but can be as late as your early 20s. Sometimes, symptoms only become noticeable if you stop taking the oral contraceptive pill. Or you might find out that you have PCOS if you see your doctor because you’re having trouble getting pregnant.
The main symptoms include:
- irregular periods – fewer than nine a year and sometimes none at all
- difficulty getting pregnant (infertility)
- being overweight or finding it hard to lose weight
- having more hair than usual, often on your top lip, chin, around your nipples, and in a line down from your tummy button
- thinning hair and losing hair on your head
- acne
- patches of dark thick skin in your armpit or around your groin or neck
PCOS is also linked with anxiety, depression, mood swings and low self-esteem.
If you have any of these symptoms, see your GP.
Diagnosis of polycystic ovary syndrome
Your GP will ask about your symptoms, your periods, and your medical history. They will look for signs of polycystic ovary syndrome (PCOS). They’ll also try to rule out conditions that can cause similar symptoms. You may need to have some tests, including:
- blood tests to measure your hormone levels and to check for other conditions
- an ultrasound scan to see if your ovaries look like you have PCOS
An ultrasound uses sound waves to build up a picture of the inside of your body. The scan may be external or internal. An external ultrasound uses a probe that the doctor moves back and forth across your tummy. An internal ultrasound uses a probe that the doctor puts into your vagina. Both will check your womb and ovaries.
Your GP will refer you to a specialist if they think you may have severe PCOS or problems with infertility.
Self-help for polycystic ovary syndrome
Lifestyle changes can help to control polycystic ovary syndrome (PCOS) symptoms. They may also improve your fertility, and can reduce your risk of long-term health problems.
Your doctor may suggest that you lose weight if you’re overweight. You may start ovulating again and having more regular periods if you lose even a small amount of weight.
You can improve your health and help to control your weight by eating a healthy, balanced diet, and exercising regularly. Changes to your diet may also help to ease symptoms. Your doctor may suggest a low GI (glycaemic index) diet. This means eating foods that cause your blood sugar levels to rise slowly.
If treatment doesn’t help with excess hair growth, you could try hair removal techniques. These include hair-removing creams, waxing, shaving, electrolysis, or laser hair removal. Or you could try bleaching products.
Treatment of polycystic ovary syndrome
There’s no cure for polycystic ovary syndrome (PCOS). But treatments can help to ease symptoms. They can also prevent complications and improve your chances of getting pregnant.
The aim of PCOS treatment will depend on your situation, and the symptoms you have.
- If you want to get pregnant, your treatment will focus on giving you the best chance of having a baby.
- If you don’t wish to become pregnant, your treatment will focus on managing your symptoms.
PCOS can increase your risk of developing long-term health problems. These include heart disease, womb cancer, and type 2 diabetes. So, part of your PCOS treatment will aim to reduce your risk of developing these conditions.
To manage your symptoms, you’ll probably need to take some of these treatments long term. But once you reach the menopause, your symptoms may improve enough for you to stop treatment. Ask your doctor for more information.
Medicines
If you are trying to have a baby, medicines used to treat infertility may help.
- Metformin may regulate your periods and help you to start ovulating again. Your doctor may suggest this if losing weight hasn’t helped.
- Fertility medicines can help your ovaries to release eggs. These include clomifene citrate or injections of female sex hormones (gonadotrophins).
If these medicines don’t work, your doctor may suggest fertility treatment such as IVF (in vitro fertilisation).
If you’re not trying to get pregnant, your doctor may suggest other treatments to manage symptoms.
- Going on the pill (oral contraceptive) can stop your ovaries producing too much testosterone. This can help to make your periods more regular. It may also help with acne.
- Your doctor may prescribe a cream called eflornithine to reduce extra hair growth.
- Co-cyprindiol is a treatment for acne and extra hair growth. It can also make your periods more regular.
- Weight loss medicines may help if lifestyle changes aren’t working.
Always read the patient information leaflet that comes with your medicines. If you have any questions, ask your pharmacist or doctor for advice.
Surgery
If medicines don’t work, your doctor may suggest you have an operation to improve your fertility. They will usually only suggest surgery if other treatments haven’t helped and will refer you to a fertility specialist.
If you’re trying for a baby, one option is keyhole surgery. This procedure is called laparoscopic ovarian drilling. The surgeon makes a small cut in your abdomen. They then put a heated probe or laser through the cut and into the ovary. They use this to destroy the ovarian tissue that produces testosterone. This changes the balance of hormones in your body, and can cause your ovaries to release eggs again.
Complications of polycystic ovary syndrome
One of the main complications of polycystic ovary syndrome (PCOS) is infertility. Your ovaries don't produce a mature egg each month, so it's more difficult to get pregnant. But if you get treatment for PCOS, you may still be able to have a baby. Losing weight may also help.
If you do get pregnant, you may be more likely to develop complications. These can include diabetes and high blood pressure. Your baby is also more likely to be born early. Your antenatal team will take extra care by giving you regular health checks.
The high insulin levels linked to PCOS increase your risk of type 2 diabetes and obesity. This can also mean that you’re more likely to develop:
- heart disease
- womb cancer
- mental health conditions such as depression and anxiety
- sleep apnoea – breathing problems during sleep that can make you extremely tired during the day
- non-alcoholic fatty liver disease
A healthy diet and exercise can significantly lower your risk of obesity and diabetes, and in turn, the chance of developing these other conditions. So, it’s important to be active and to eat well. Talk to your doctor if you’re worried about complications or getting pregnant.
Worried about your gynaecological health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0370 218 8122
PCOS can have several different symptoms caused by hormone imbalances. As well as irregular periods, you may gain weight, have excess body hair or acne. It can also affect your mood and increase the risk of depression. For more information, see the symptoms section.
Polycystic ovary syndrome is likely to be caused by a combination of lifestyle factors and the genes you’ve inherited. Although it’s not possible to cure it, changes to your lifestyle may help to reduce symptoms. See our section on self-help for more information.
If you have polycystic ovary syndrome (PCOS) you might have difficulty getting pregnant. Irregular periods, fewer periods, or none at all can make it more difficult to conceive. If you’re having difficulty conceiving, treatment for PCOS may help you to have a baby. See our section on complications for more information.
Polycystic ovary syndrome (PCOS) is likely to be caused by a combination of things. But your risk may be higher if your mother or sister has the condition. We now know of some genes that are linked to PCOS. See the section on causes of PCOS for more information.
Benefits of exercise
Not only does regular exercise help you manage your weight and reduce your risk of developing diseases, it can help prevent and treat mental health problems
How to start exercising
We should all be getting active – and it may be easier than you think. Here we give you tips and advice for getting started
Tips for a healthy and well-balanced diet
A healthy, well-balanced diet involves eating foods from a variety of food groups to get the nutrients that your body needs to function.
Other helpful websites
Discover other helpful health information websites
Did our Polycystic ovary syndrome information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers. The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Polycystic Ovary Syndrome (PCOS). MSD Manual. msdmanuals.com, last reviewed January 2023
- Polycystic ovary syndrome. NICE Clinical Knowledge Summary. cks.nice.org.uk, last revised February 2022
- Polycystic ovary syndrome. BMJ Best Practice. bestpractice.bmj.com, last updated April 2023
- Ovary Anatomy. Medscape. emedicine.medscape.com, last updated September 2018
- Oxford Handbook of General Practice. Oxford Medicine Online. academic.oup.com, published June 2020
- Polycystic ovary syndrome (PCOS): what it means for your long-term health. Royal College of Obstetricians and Gynaecologists. rcog.org.uk, accessed April 2023
- PCOS. Medline Plus. medlineplus.gov, last updated January 2020
- Luteinizing Hormone (LH) Levels Test. Medline Plus. medlineplus.gov, last updated December 2020
- Polycystic Ovarian Syndrome. Medscape. emedicine.medscape.com, last updated September 2019
- Polycystic ovary syndrome. Patient. patient.info, last updated March 2021
- Polycystic Ovary Syndrome (PCOS) and diet: Food Fact Sheet. British Dietetic Association. bda.uk.com, last updated May 2022
- Hirsutism. NICE Clinical Knowledge Summary. cks.nice.org.uk, last reviewed July 2020
- Co-cyprindiol. NICE British National Formulary. bnf.nice.org.uk, accessed May 2023
- Polycystic ovary syndrome: metformin in women not planning pregnancy. National Institute for Health and Care Excellence. nice.org.uk, published February 2013
- Orlistat. NICE British National Formulary. bnf.nice.org.uk, accessed May 2023
- Liz Woolf, Freelance Health Editor



