Anal fissure procedures
Your health expert: Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon
Content editor review by Pippa Coulter, Freelance Health Editor, June 2023
Next review due June 2026
Procedures for anal fissures include botulinum toxin injections and a type of surgery called a sphincterotomy. Your doctor may suggest you have one of these procedures if your anal fissure isn’t healing on its own or with medical treatments.
About treatments for anal fissure
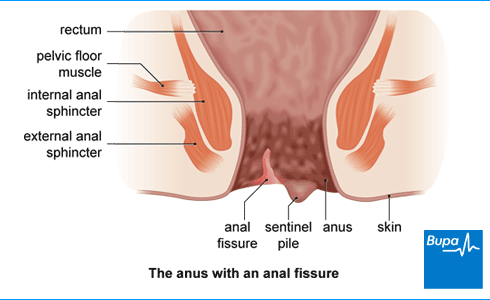
An anal fissure is a small tear or split in the skin around your anus (the opening of your bottom). It can cause severe pain and bleeding when you have a poo.
Anal fissures often heal within 6 to 8 weeks using self-help measures. These include increasing your fibre and fluid intake or taking medicines to soften your poo. Taking over-the-counter painkillers and warm baths can help to ease pain. Your doctor may also prescribe an ointment or cream. If you’ve tried these measures for 6 to 8 weeks and the fissure doesn’t heal, your doctor may suggest a procedure.
If you have an anal fissure, the sphincter muscles around your anus spasm and tense up. This reduces the blood supply to the area, which stops the tear from healing properly. Anal fissure surgery aims to relax your sphincter muscles to help the fissure heal. Procedures for anal fissures include botulinum toxin injections, lateral internal sphincterotomy and anal advancement flaps.
Deciding on treatment
Your doctor will talk to you about which procedure might be suitable for you, and explain what’s involved. They’ll discuss the possible benefits and risks of the procedure.
This is your chance to ask questions so that you understand what will happen. Take your time to think about your options before deciding. Whether or not you have anal fissure surgery is your choice. You might decide to carry on trying other treatments.
If you do decide to go ahead with a procedure, you’ll be asked to sign a consent form (sometimes called an agreement form).
The main procedures are covered in the sections below.
Botulinum toxin injections
If your fissure hasn’t healed with ointment or cream you’re likely to be offered a Botox injection. Botulinum toxin (Botox) is a medicine that can help stop muscle spasms. When it’s used for the treatment of anal fissures, it’s injected into the sphincter muscle in your bottom. This helps the muscles to relax, allowing the fissure to heal naturally.
You’ll have Botox injections for anal fissure in a hospital operating theatre, under general anaesthesia. This means you’ll be asleep for the procedure.
Your surgeon may suggest having a procedure called a fissurectomy alongside Botox injections. This involves cutting away the damaged skin from around the anal fissure.
How well does it work?
Studies show that fissures heal in around 6 to 8 out of 10 people who have Botox injections. It usually takes 4 to 8 weeks after having the injection for the fissure to heal. It might be that your fissure would have healed during this time anyway. You might need a second set of injections a few months after the first one for the fissure to heal completely. It’s possible for your fissure to come back or to get another fissure after Botox injections, sometimes years later.
What are the risks?
There can be side-effects of Botox injections. Between 1 and 2 in 10 people have temporary problems controlling their bowels, including passing wind and going for a poo. This may last a few weeks.
Very rarely, Botox can spread to other parts of your body. This may cause weakness in your muscles and difficulties with breathing or swallowing. Contact your doctor or the hospital where you had the procedure if you experience any of these symptoms.
Lateral internal sphincterotomy
This procedure involves cutting the sphincter muscles around your anus to release the tension in the muscles. This lets the fissure heal. Your doctor will usually only suggest this after you’ve tried other treatments first, including Botox. The operation is done under general anaesthesia, which means you’ll be asleep. Usually, you can go home the same day.
The procedure can be done in two ways. In an open sphincterotomy, your surgeon makes a small cut in your skin so they can see the sphincter muscle. The cut is usually left open to heal. In a closed sphincterotomy, your surgeon passes a blade under your skin to reach and cut the muscle.
How well does it work?
Lateral internal sphincterotomy is the most effective type of surgery for anal fissure. Between 9 and 10 out of every 10 people who have this surgery find that their fissure heals. This is usually within 8 weeks of treatment. Your fissure may come back again after this surgery but this is less likely than with Botox injections.
What are the risks?
The main complication after this type of surgery is incontinence. Up to 3 in 10 people may have some problems controlling their bowels at first, including when they poo or pass wind. These problems are usually minor and get better over time, but for around 2 in 100 people, they can be permanent.
Other possible complications include the following.
- Bleeding from the area around your anus or under your skin (a haematoma).
- An infection, which causes an abscess. If this happens, it’s usually treated by draining the abscess or taking antibiotics.
- An anal fistula. This is a small channel that develops between the inside of your bottom and your skin. It can usually be treated with a small operation.
Anal advancement flaps
In this procedure, your surgeon takes a piece of healthy skin and stitches it in place to replace the damaged skin in the fissure. This is only suitable for a small group of people. The treatment is less effective than a lateral internal sphincterotomy but is less likely to cause incontinence. Your surgeon may suggest it if you keep getting fissures or if you’re more likely to develop incontinence after surgery.
Aftercare following an anal fissure procedure
Anal fissure procedures are done under general anaesthesia as a day-case procedure in a hospital. This means you have the procedure and go home on the same day.
After your procedure, you’ll need to rest until the effects of the anaesthetic have worn off. You may also need pain relief to help ease any discomfort. You should be able to go home as soon as you feel ready. Make sure someone can take you home.
A general anaesthetic can affect your co-ordination and make it difficult to think clearly. You shouldn’t drive, drink alcohol, operate machinery or make any important decisions for 24 hours after your anaesthetic. A friend or relative should stay with you for the first 24 hours while the anaesthetic wears off.
Your nurse will give you some advice about caring for your healing wounds before you go home.
You may also be given a date for a follow-up appointment to check that your wound and fissure are healing properly.
Anal fissure surgery recovery
It takes a day or two to recover from having Botox injections. It may take a week or two to recover after a sphincterotomy or fissurectomy.
You’ll have some pain and discomfort after any type of anal fissure surgery. You’ll be given painkillers and medicines to take at home. These will be to soften your poo. You should also drink plenty of fluids and eat foods that are high in fibre. This will help to keep your poo soft, making it more comfortable when you go to the toilet. High-fibre foods include fruit and vegetables, wholegrain breads, and cereals.
It’s important to keep your bottom clean and dry. Your doctor or nurse will give you some advice about this before you leave hospital. They may suggest taking a bath or shower every time you have had a poo. Or, it may be best to gently clean the area with damp cotton wool. You might notice blood in your poo or on the toilet paper for up to 10 days after your operation. Some people also get mucus from their bottom for a few days.
The recovery time varies from person to person. Most people feel well enough to return to their usual activities within a few days.
If you develop severe pain, bleeding or a fever, get medical advice. Contact your GP or the hospital where you had the procedure.
Follow-up after anal fissure procedures
You’ll normally have an appointment after your anal fissure procedure to check if it’s healed. If your fissure hasn’t healed after Botox injections, your doctor may suggest trying the same treatment again. Or they may suggest a sphincterotomy operation or anal advancement flaps. If your fissure still doesn’t heal or comes back again, your surgeon may suggest some tests to check the results of the surgery. These may include an ultrasound scan and tests to see how well your sphincter muscle is working.
Your doctor may also investigate whether or not there is an underlying cause for the fissure. Medical conditions like Crohn’s disease and some sexually transmitted infections can cause an anal fissure. Treating any underlying conditions may help to heal the fissure.
Your doctor may suggest trying the same treatment again or another type of treatment. This will depend on your individual situation.
Yes, you should expect some pain and discomfort around your anus after anal fissure surgery. You can help soften your poo by drinking plenty of fluids and eating foods that have fibre in them. Also make sure you take any laxative that your surgeon has prescribed. This will make things more comfortable when you need to poo. For more information, see our section on recovery.
Your doctor may recommend another procedure. If you previously had Botox injections, they may suggest trying more injections. Or they may suggest a sphincterotomy operation. If this doesn’t work, they will usually do some tests to check for any underlying conditions that could be causing your anal fissure. For more information, see our section on follow-up.
Surgery can permanently cure an anal fissure for some people. But in others, it may not heal the fissure or the fissure may come back after some time. This is less common after a sphincterotomy than Botox injections. If your fissure comes back, you may be able to have more treatment. For more information, see our section on treatments and our sections on individual procedures.
It can take up to 8 weeks after surgery for your anal fissure to heal. This may depend on the type of procedure you have. It may take less time for some people. Sometimes, you may need more treatment for your fissure to fully heal. For more information, see our section on follow-up.
Anal fissure
An anal fissure is a small tear or ulcer (open sore) in your skin around the opening of your bottom.
General anaesthesia
General anaesthesia is when medication is given to make you temporarily unconscious during an operation, so don't feel pain or other sensations.
How to take care of your surgical wound
Preparing for your surgery and recovery
We give lots of advice and tips on how to prepare for your surgery, and what you can do to help yourself recover well afterwards.
Did our Anal fissure procedures information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Chronic anal fissure: botulinum toxin type A injection. Information for the public. National Institute for Health and Care Excellence (NICE). nice.org.uk, published 25 June 2013
- Cross KLR, Massey EJD, Fowler AL, et al. The management of anal fissure: ACPGBI Position Statement. Colorectal Dis 2008; 10:1–7
- Anal fissure. BMJ Best Practice. bestpractice.bmj.com, last reviewed 22 April 2023
- Newman M, Collie M. Anal fissure: diagnosis, management, and referral in primary care. Br J Gen Pract 2019; 69(685):409–10. doi: 10.3399/bjgp19X704957
- Anal fissure. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last reviewed April 2021
- Boland PA, Kelly ME, Donlon NE, et al. Management options for chronic anal fissure: a systematic review of randomised controlled trials. Int J Colorectal Dis 2020; 35(10):1807–15. doi: 10.1007/s00384-020-03699-4
- Good surgical practice. The Royal College of Surgeons. www.rcseng.ac.uk, published September 2014
- Soltany S, Hemmati HR, Toussy JA, et al. Therapeutic properties of botulinum toxin on chronic anal fissure treatment and the patient factors role. J Family Med Prim Care 2020; 9(3):1562–66. doi: 10.4103/jfmpc.jfmpc_944_19
- Personal communication, Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon, 15 June 2023
- Brisinda G, Chiarello MM, Crocco A, et al. Botulinum toxin injection for the treatment of chronic anal fissure: uni- and multivariate analysis of the factors that promote healing. Int J Colorectal Dis 2022; 37(3):693–700. doi: 10.1007/s00384-022-04110-0
- Colorectal surgery. Surgery for fissure – in-ano. Oxford Handbook of Operative Surgery. Oxford Academic. academic.oup.com, published online May 2017
- Anal fissure. Medscape. emedicine.medscape.com, updated 29 March 2023
- You and your anaesthetic. Royal College of Anaesthetists, www.rcoa.ac.uk, published February 2020
- Caring for someone recovering from a general anaesthetic or sedation. Royal College of Anaesthetists. www.rcoa.ac.uk, published November 2021
- Surgical wounds – principles of wound management. Oxford Handbook of Adult Nursing. Oxford Academic. academic.oup.com, published online June 2018
- Lateral anal sphincterotomy. The Association of Coloproctology of Great Britain and Ireland. www.acpgbi.org.uk, accessed 23 May 2023
- Fibre. British Dietetic Association. www.bda.uk.com, published April 2021



