Coeliac disease
- Dr Derek Chan, Consultant Physician and Gastroenterologist
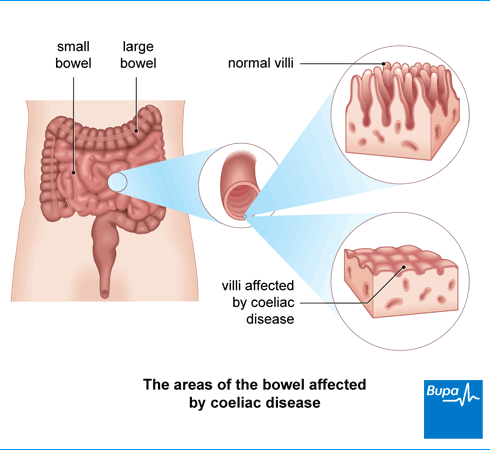
Coeliac disease is an autoimmune condition that causes your body to react to gluten, a protein found in wheat, barley and rye. This reaction causes damage to the lining of your small bowel (intestine), which then can’t absorb nutrients properly. It can sometimes cause coeliac disease symptoms such as diarrhoea, tummy cramps and bloating.
About coeliac disease
Coeliac disease isn’t the same as a food allergy or food sensitivity, it’s an autoimmune condition. This means your body’s immune system mistakenly attacks your own healthy tissue. If you have coeliac disease, this reaction happens when you eat a protein called gluten. Your immune system mistakes gluten for something harmful. Gluten is a protein found in wheat, barley and rye. This means it is found in foods such as bread, cereals and pasta.
When your immune system attacks gluten, it damages the lining of your small bowel (intestine). The lining of your small bowel is made up of tiny finger-like projections called villi. In coeliac disease, your villi become damaged and flattened. This stops your small bowel fully absorbing nutrients in your food.
It’s thought that 1 in 100 people have coeliac disease. Most people develop coeliac disease as a child or in midlife (between your 40s and 60s) but you can get it at any age. If you have it, you’ll need to follow a life-long, gluten-free diet. This stops coeliac disease symptoms for most people.
Causes of coeliac disease
Doctors aren’t yet sure what causes coeliac disease. It may run in families – almost 1 in 10 people who have coeliac disease have a sibling or parent who also has it. But having a relative with coeliac disease doesn’t necessarily mean that you’ll get it.
You’re more likely to get coeliac disease if you have another autoimmune condition, such as type 1 diabetes or autoimmune thyroid disease.
Symptoms of coeliac disease
You might not get any coeliac disease symptoms. You may only find out when your doctor checks you because you have another, related medical condition such as a vitamin deficiency.
If you do have coeliac disease symptoms, they can vary widely. Coeliac disease symptoms include:
- diarrhoea – which may smell especially unpleasant
- a bloated tummy (abdomen)
- tummy cramps
- wind
- unexplained weight loss
- feeling very tired all the time (fatigue)
- being sick (vomiting)
- constiptation
Signs of coeliac disease are similar to irritable bowel syndrome (IBS). So if you have IBS, your GP may test you for coeliac disease to see if this is causing your symptoms.
If you’re not absorbing your food properly, you may be short of vitamins and minerals. This can lead to you developing conditions such as anaemia and osteoporosis.
Young children with coeliac disease may find it difficult to gain weight. They may grow more slowly than other children. They may also be more irritable than usual.
If you have these symptoms, it doesn’t necessarily mean you have coeliac disease. But it’s best to get things checked out by your GP.
Diagnosis of coeliac disease
Diagnosis of coeliac disease involves:
- a blood test
- a biopsy of your small intestine
Blood test
When you see your GP, they’ll ask about your symptoms and your family’s medical history. If they think you might have coeliac disease, your GP will offer you a coeliac disease blood test. This will look for certain antibodies that are present in people with coeliac disease.
If the coeliac disease blood test shows that you have these antibodies, your GP will refer you to a gastroenterologist. This is a doctor who specialises in identifying and treating conditions that affect the digestive system. If your blood test is negative but you keep having symptoms, your GP may still refer you.
Intestinal biopsy
Your gastroenterologist may suggest you have an endoscopy (gastroscopy) to take small bowel biopsies. Your doctor will use a narrow, flexible, tube-like telescopic camera called an endoscope. They’ll pass this through your mouth down to your stomach and on to your small bowel. They’ll then take a small sample (biopsy) of the lining of your bowel.
The sample will be sent to a laboratory to look for damage to your bowel. Your doctor will explain the procedure to you and discuss ways to make it as comfortable as possible. You can find out more about this type of procedure in our gastroscopy topic.
Important information about eating gluten and testing
It’s very important that you’re still eating gluten when you have these tests. If you’ve already changed to a gluten-free coeliac disease diet, your tests may appear normal even if you have coeliac disease. Aim to eat some gluten in more than one meal every day for at least six weeks before you’re tested.
GP Subscriptions – Access a GP whenever you need one for less than £20 per month
You can’t predict when you might want to see a GP, but you can be ready for when you do. Our GP subscriptions are available to anyone over 18 and give you peace of mind, with 15-minute appointments when it suits you at no extra cost.
Treatment of coeliac disease
The only treatment for coeliac disease is to follow a life-long, strict gluten-free diet. You may find your symptoms improve within a week or two once you’ve cut out gluten completely.
Your doctor will refer you to a specialist dietitian. They’ll offer you lots of support and practical help to help you manage your condition. They may suggest you contact a coeliac disease charity, which can give you lots of practical advice. For more information, see our section on other helpful websites.
Avoiding gluten
Gluten is found in foods made with wheat, barley or rye. So you’ll need to avoid products such as:
- bread
- pastry
- cakes
- pasta
- pizza bases
- biscuits
Gluten is also found where you may not expect it – for example, breakfast cereals and processed foods such as sausages, soups and sauces. Most beers also contain gluten. Oats may be contaminated with gluten, so you need to buy gluten-free oats. You’ll need to check the labels on foods. Gluten should be listed on products because it’s an allergen.
Foods that are labelled as gluten-free or that have the Crossed Grain Symbol are generally safe for most people with coeliac disease to eat. You can find gluten-free bread, biscuits and pasta in most supermarkets or health food shops.
If you’re eating out and the menu doesn’t say whether or not the food contains gluten, just ask. If in doubt, it’s safer not to eat something you’re unsure about.
Understandably, many people find it hard to stick to a strict gluten-free diet. But it really is important for your health. Nine out of 10 people with coeliac disease who stick to a gluten-free diet find that their symptoms go away.
If you have coeliac disease, your dietitian may advise you to take some vitamin and mineral supplements (for example, calcium and vitamin D).
Eating gluten by accident
It can be difficult to follow a gluten-free diet and mistakes happen, especially when you’re just starting. If you eat gluten, you may get some coeliac disease symptoms a few hours after you eat. These could last for a few hours to several days.
But everyone with coeliac disease is different and you may find you don’t have any symptoms at all. If you make the odd mistake, it won’t cause any lasting damage to your bowel. But if you have coeliac disease, it’s important to always check what you’re eating and follow a gluten-free coeliac diet.
Regular health checks
Coeliac disease is a lifelong condition so you’ll need regular check-ups. These are usually once a year, and may be with your pharmacist, specialist nurse, dietitian or doctor.
At your check-up, they’ll ask you about any symptoms you have and how you’re getting on with your gluten-free diet. Children and teenagers may have their height measured to make sure they’re growing properly. You may need blood tests to check your health and to see if your body is absorbing enough nutrients.
Because of the risk of getting osteoporosis, from time to time your GP may recommend that you have a dual X-ray absorptiometry (DXA) scan. This will check the density of your bones.
Having coeliac disease can mean you’re less able to fight infections. Your GP will suggest you have the annual flu vaccine and the pneumococcal vaccine that protects against some types of pneumonia. If they recommend you have other vaccinations, they’ll explain why.
Complications of coeliac disease
Coeliac disease may lead to a range of potential health problems. But you can greatly reduce your risk of developing these complications if you stick to a gluten-free diet.
Complications of untreated coeliac disease include the following.
- Illness caused by lack of nutrients, including deficiency in iron (causing anaemia) and other vitamins or minerals.
- Osteoporosis, this is when your bones become weakened and are more likely to break.
- Reduced growth, and delayed puberty in children.
- Reduced fertility in both men and women.
- A skin problem called dermatitis herpetiformis, where itchy blisters form on your skin.
- A small, increased risk of developing certain cancers of the digestive tract and some kinds of lymphoma.
The most common coeliac disease symptoms are diarrhoea, tummy cramps, bloating and feeling very tired all the time. Other coeliac disease symptoms include unexplained weight loss and wind. The severity of the symptoms can vary widely. Some people don’t get any symptoms at all.
For more information, see our section on symptoms of coeliac disease.
If you have coeliac disease, you can’t eat any foods that contain gluten. This means anything that contains wheat, barley or rye. Food labels should tell you if there’s gluten in them, so you should get into the habit of reading these carefully. A dietitian can give you advice about what to eat, and you can get more information from Coeliac UK.
Coeliac disease is usually diagnosed in a two-step process. First, you have a blood test to check if you have antibodies found in people with coeliac disease. Sometimes coeliac disease is diagnosed just on blood testing; particularly in children if the antibody level is very high. The diagnosis can be confirmed by having an intestinal biopsy.
For more information, see our section on diagnosis of coeliac disease.
For most people, coeliac disease isn’t serious if they eat a gluten-free diet. But coeliac disease can cause some complications which can be serious. These include illness from vitamin deficiencies such as anaemia, and osteoporosis. There’s also a small risk of developing certain cancers of the digestive tract. But you can greatly reduce your risk of developing these complications if you stick to a gluten-free diet.
People can develop coeliac disease at any time in their lives. The main coeliac disease trigger is consuming gluten. There are theories for other triggers of coeliac disease. These include an infection in part of your digestive system, and taking certain medicines. Gastrointestinal surgery has also been suggested to reveal undiagnosed coeliac disease. But there’s no scientific evidence to know for sure. There are probably lots of people who have the condition, but have never been diagnosed because not everyone gets symptoms.
Gastroscopy
A gastroscopy is a procedure that allows a doctor to look inside your oesophagus , your stomach and part of your small intestine.
Vitamins and minerals
Different vitamins and minerals do different things: some help your body to digest food while others build strong bones
Did our Coeliac disease information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Coeliac disease. BMJ Best Practice. bestpractice.bmj.com, last reviewed 9 September 2024
- Causes. Coeliac UK. www.coeliac.org.uk, accessed 9 October 2024
- Celiac disease. MSD Manuals. msdmanuals.com, reviewed/revised March 2023
- Coeliac disease. Patient. patient.info, last updated 22 December 2021
- Posner EB, Haseeb M. Celiac disease. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 8 August 2023
- About coeliac disease. Coeliac UK. www.coeliac.org.uk, accessed 10 October 2024
- Pediatric celiac disease (sprue). Medscape. emedicine.medscape.com, updated 7 July 2023
- Coeliac disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised May 2020
- Coeliac disease: Recognition, assessment and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published September 2015
- The gluten free diet. Coeliac UK. www.coeliac.org.uk, accessed 10 October 2024
- Rachael Mayfield-Blake, Freelance Health Editor



