Fundoplication
- Mr Peter Lamb, Consultant Upper Gastrointestinal and General Surgeon
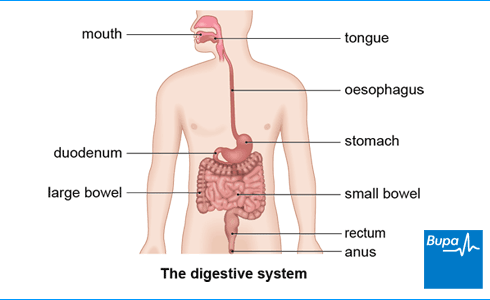
Fundoplication is an operation to treat gastro-oesophageal reflux disease (GORD). It involves wrapping the top part of your stomach around your lower oesophagus (the tube that carries food from your mouth to your stomach).
About GORD and fundoplication
Gastro-Oesophageal Reflux Disease (GORD) is a condition where the contents of your stomach regularly leak back into your oesophagus. Your stomach contents are acidic, so they can irritate the lining of your oesophagus when they come into contact with it. This can cause symptoms such as heartburn – when you get a burning feeling rising up from your stomach towards your neck.
Your doctor will usually suggest you try indigestion medicines called proton pump inhibitors and make changes to your lifestyle to treat GORD. These include changes to your diet and losing any excess weight if you need to. For most people, these measures control the symptoms of GORD well. But sometimes, you may find that proton pump inhibitors don’t fully control your symptoms or that you can’t take them for long because of side-effects. If this happens to you, fundoplication surgery could be an option.
If your doctor thinks you may benefit from fundoplication surgery, they’ll refer you to a surgeon for an assessment. Fundoplication is an effective procedure for many people and means they no longer need to take medicines for GORD.
A hiatus hernia, can cause GORD. It’s when part of your stomach slides up into your chest. If you have a hiatus hernia, your surgeon will repair it as part of the fundoplication operation.
Types of fundoplication
There are different ways of doing a fundoplication. The two most common are described below.
- Nissen’s fundoplication. In this method, your surgeon will wrap the top part of your stomach all the way around the lower part of your oesophagus.
- Partial fundoplication. In this type, your surgeon will wrap the top of your stomach part of the way around your oesophagus. This may be around the front (anterior fundoplication) or the back (posterior or Toupet fundoplication).
Fundoplication is usually done as keyhole (laparoscopic) surgery. This means it’s done through very small cuts (incisions) in your skin. Occasionally, open surgery is necessary. This means your surgeon will make a single, bigger cut in your tummy (abdomen).
Preparation for fundoplication
Deciding on surgery
At your first appointment, your surgeon will discuss exactly what’s involved in a fundoplication procedure so you can decide if it’s right for you. This will include any potential complications and what to expect afterwards. Be sure to ask your surgeon any questions you have and take time to make your decision. If you decide to go ahead, you’ll be asked to sign a consent form, so it’s important to make sure you feel properly informed.
Getting ready for surgery
Your surgeon will explain how to prepare for your operation. If you smoke, your surgeon will advise you to stop. Smoking increases your risk of getting a chest and wound infection, which can slow your recovery.
Fundoplication is done under general anaesthesia, which means you’ll be asleep during the operation. You’ll need to stop eating and drinking for some time before your operation. Your surgeon will give you clear instructions about this. It’s important to follow their advice.
You may need to stay in hospital overnight after your surgery, so make any necessary preparations. Your stay in hospital is likely to be longer if you have open surgery. Sometimes, you may be able to go home on the day of your procedure. If so, you’ll need someone to drive you home and stay with you overnight.
On the day
On the day of your procedure, your surgeon will meet with you to check you are well and still happy to go ahead. The staff at the hospital will do any final checks and get you ready for surgery. You may need to wear compression stockings or have an injection of an anticlotting medicine to help prevent deep vein thrombosis (DVT).
Fundoplication procedure
In keyhole surgery, your surgeon will insert small instruments and a tube-like camera through small cuts in the skin of your tummy. If you’re having open surgery, your surgeon will make one long cut from the bottom of your breastbone down to just above your tummy button. Occasionally your surgeon may need to change from keyhole to open surgery during the procedure.
If you have a hiatus hernia, your surgeon will repair this first. To do the fundoplication, your surgeon will wrap the top part of your stomach around the lower end of your oesophagus and sew this into place. They may wrap your stomach all the way around your oesophagus (Nissen’s fundoplication) or part of the way round (partial fundoplication).
At the end of the operation, your surgeon will close the cuts in your skin with stitches. These may be dissolvable. This means they are made from a material that your body can break down and absorb. They’ll eventually disappear on their own and won’t need to be removed. Ask your surgeon how long it will take for them to dissolve.
Aftercare following fundoplication
You’ll need to rest until the effects of the anaesthetic have passed. You may need pain relief to help with any discomfort as the anaesthetic wears off. Once you’re ready, your nurses will encourage you to get up and move around. This will help to prevent complications. You’ll be able to drink something a few hours after your operation, but usually you won’t be able to eat anything until the following day.
Sometimes you can go home on the day of your operation, but you may need to stay overnight in hospital. If you’ve had open surgery, you’ll usually need to stay in hospital for longer – for between two and five days.
Your nurse will give you some advice about caring for your healing wounds before you go home. They’ll also give you some information about what you can eat and drink while you recover, and a follow-up appointment date.
If your surgeon used clips or non-dissolvable stitches, you’ll need to have these removed after about seven to 12 days.
Looking for prompt access to quality care?
With our health insurance, if you develop new conditions in the future, you could get the help you need as quickly as possible, from treatment through to aftercare.
To get a quote or to make an enquiry, call us on 0800 600 500∧
Recovering following fundoplication
It can take up to six weeks for any initial discomfort and side-effects after fundoplication to settle down. But the time it takes to fully recover can vary from person to person. Recovery tends to be quicker after keyhole surgery than open surgery.
Don’t lift anything heavy for the first month or so after your operation. If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen.
Side-effects of fundoplication
Side-effects of fundoplication include:
- feeling sick, which usually only lasts for a short time
- difficulty swallowing for the first few days or sometimes weeks
- bloating and discomfort after eating
Follow any advice your hospital gives you about what to eat while you recover. You can usually eat smaller portions of soft foods. You’ll need to take your time when you eat, and don’t have very solid foods such as meat, bread and pasta for around four to six weeks. It’s best not to have fizzy drinks because these can increase gas in your stomach and make any bloating worse.
Complications of fundoplication
Complications are when problems occur during or after the operation. Possible complications of fundoplication include the following.
- Rarely, your stomach, oesophagus or other nearby organs such as your spleen could be damaged during the operation. If you have severe pain or are constantly being sick, contact your hospital straight away.
- Difficulties with swallowing that continue for longer than normal. If you’re still having problems after around 12 weeks, you may need an examination to check whether or not everything is OK. You may need another operation.
- Bloating and wind is common but can be more severe in some people. Your doctor may be able to give you medicines to help with this. Rarely, you may need another operation.
- You may find that the symptoms of GORD come back after your operation. If this happens, you might need a second operation.
Alternatives to fundoplication
Your doctor will only offer you a fundoplication operation if you’ve already tried lifestyle measures and medicines. The main alternative to having the operation is to continue taking medicines (such as proton pump inhibitors) long-term.
Some surgeons perform a keyhole procedure for GORD that involves inserting a ring of magnetic beads around your lower oesophagus (LINX procedure). This allows you to swallow food, but keeps your oesophagus closed afterwards to prevent acid leaking back up from your stomach. It’s only available in certain hospitals at the moment.
Side-effects after fundoplication surgery may include mild pain and discomfort. It’s quite common to feel sick and have some trouble swallowing at first. You might have some bloating and increased wind too. Most of these problems improve over a few weeks.
For more information, see our section on side-effects of fundoplication.
Fundoplication surgery can be major surgery but the risk of serious complications afterwards is small. You’ll need to have a general anaesthetic. And you’re likely to have some discomfort for a few weeks after the procedure. You’ll have to take care for a while after your surgery – for example, don’t lift anything heavy for the first month or so after your operation.
The difference between fundoplication and Nissen’s fundoplication is the technique your surgeon will use to do the procedure. Nissen’s fundoplication means wrapping your stomach all the way around your oesophagus. Other methods involve wrapping your stomach part of the way around.
For more information, see our section on types of fundoplication
It can take up to six weeks to recover from fundoplication, and for any side-effects to settle down. But this varies from person to person. Recovery tends to be quicker after keyhole surgery than open surgery. And you’ll recover better if you don’t smoke because smoking increases your risk of getting a chest and wound infection, which can slow your recovery.
For more information, see our section on recovering following fundoplication.
Fundoplication surgery is an effective procedure and should resolve symptoms that are caused by GORD, such as vomiting. But there’s always a chance that the symptoms of GORD come back after your operation. If this happens, you might need a second operation.
Did our Fundoplication information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
General anaesthesia
General anaesthesia is when medication is given to make you temporarily unconscious during an operation, so don't feel pain or other sensations.
Hiatus hernia
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Dyspepsia – proven GORD. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2023
- Gastro-oesophageal reflux disease. BMJ Best Practice. bestpractice.bmj.com, last reviewed 2 February 2024
- Hiatus hernia. BMJ Best Practice. bestpractice.bmj.com, last reviewed 2 February 2024
- Seeras K, Bittar K, Siccardi MA. Nissen fundoplication. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 17 July 2023
- Open Nissen fundoplication. Medscape. emedicine.medscape.com, updated 21 November 2022
- Parker J, Mortimore G. Consent in surgery. Br J Nurs 2023; 32(12) doi: https://doi.org/10.12968/bjon.2023.32.12.588
- Preparing your body. Royal College of Anaesthetists. www.rcoa.ac.uk, accessed 2 March 2024
- You and your anaesthetic. Royal College of Anaesthetists. www.rcoa.ac.uk, published April 2023
- Laparoscopic Nissen fundoplication. Medscape. emedicine.medscape.com, updated 5 May 2022
- Hiatus hernia. Patient. patient.info, last updated 14 April 2020
- Venous thromboembolism in over 16s: Reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 13 August 2019
- Wound closure technique. Medscape. emedicine.medscape.com, updated 22 June 2021
- Laparoscopic insertion of a magnetic ring for gastro-oesophageal reflux disease. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 11 January 2023
- Khan AZ, Tønseth KA, Koidl A, et al. Suture materials. Tidsskr Nor Laegeforen 2023; 143. doi: 10.4045/tidsskr.22.0708
- Rachael Mayfield-Blake, Freelance Health Editor



