Indigestion
- Dr Lewis Caplin, Lead Physician at Bupa
- Atiya Henry, Health Content Editor
Indigestion is a term used to describe a range of symptoms, including pain or discomfort in your upper abdomen. It’s also known as dyspepsia. Indigestion is very common. It’s usually something you can manage yourself with lifestyle changes or over-the-counter medicines.
About indigestion
Around 4 in every 10 people in the UK get indigestion every year. It can affect everyone differently, but indigestion symptoms often include pain or a burning feeling just under your ribs or higher up in your chest.
You may notice certain things trigger your indigestion symptoms – for example, eating fatty foods or drinking alcohol or coffee. But some people get indigestion symptoms which aren’t related to eating or drinking, at any time.
Indigestion can be caused by many things. Certain conditions can be associated with indigestion, but it’s often not possible to say what’s causing it.
Causes of indigestion
Often, it’s not possible to find an underlying cause for your indigestion. Your symptoms could be due to many things, including increased sensitivity in your bowel or acid irritating your stomach lining. You may also develop indigestion after having an infection.
Sometimes, doctors identify an underlying cause for your indigestion. These may include the following.
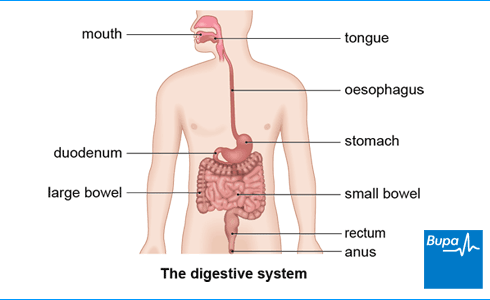
- Gastro-oesophageal reflux disease (GORD). This is when acid leaks out of your stomach and up into your food pipe (oesophagus). Certain factors may make you more likely to develop GORD. These include being obese, being pregnant, or having a hiatus hernia. Smoking, alcohol, and certain foods can trigger GORD too.
- Peptic ulcer. This is a break in the lining of your stomach or duodenum (part of your small bowel). Peptic ulcers are often associated with Helicobacter pylori (H. pylori) infection. Certain medicines, including non-steroidal anti-inflammatory drugs (NSAIDs) and aspirin can increase risk of peptic ulcers. Smoking, alcohol, and stress can also be factors.
- Stomach (gastric) cancer. This is a rare cause of indigestion, but it’s something your doctor may need to investigate.
Pregnancy and indigestion
You’re more likely to get indigestion and heartburn during pregnancy. Your hormones can make the band of muscle between your oesophagus and stomach more relaxed. This means some of your stomach contents can come back up into your oesophagus (called reflux). You may also have indigestion because your growing baby in your womb (uterus) presses against your stomach.
Symptoms can start at any stage of pregnancy. They’ll usually get better with lifestyle changes and over-the-counter medicines, and go away once you’ve had your baby. If you have indigestion or heartburn symptoms in pregnancy, speak to your midwife, pharmacist or GP.
Symptoms of indigestion
The term indigestion refers to lots of different symptoms. If you have indigestion, you may have all these symptoms or just a few:
- pain, fullness, or discomfort in your upper abdomen
- a burning feeling in your chest (heartburn)
- wind or bloating
- feeling or being sick
- feeling full quickly when you eat
You won’t usually need to see your GP if your symptoms are mild. But if your symptoms don’t go away within a few weeks, are getting worse, or self-help measures aren’t working, contact your GP.
There are times when you should see your GP straightaway if you have indigestion. These include if you:
- are over 55, and have also lost weight without trying or are being sick regularly
- are finding it difficult to swallow
- have blood in your vomit or poo
- notice your poo suddenly turns black in colour
Occasionally, a heart attack can cause indigestion-like symptoms. Call for emergency help if you have sudden pain in your chest or upper abdomen. During a heart attack, the pain may also spread to your arms, shoulder, neck or jaw. You may have other symptoms too such as sweating, shortness of breath, and feeling or being sick.
Diagnosis of indigestion
You won’t usually need to have indigestion diagnosed by a doctor. But if you do see your GP, they’ll want to ask you about your symptoms and medical history.
They’ll ask if anything makes your symptoms better or worse (such as alcohol, exercise, or certain foods). You may find it helps if you keep a diary before you see your GP to record this information.
Your GP may want to examine you by feeling your tummy and sometimes they may ask you to have a blood test. This is to help check for any other underlying health conditions you may have that may be causing your indigestion.
Food and symptoms diary
Your indigestion may be triggered by certain foods and drinks, such as chocolate, alcohol, coffee and spicy or fatty foods. It may also be triggered by smoking, eating close to bedtime, stress, and other lifestyle habits. Keeping a diary of what you eat and do every day may help to identify anything that could be triggering your indigestion or making it worse.
Download a PDF version of Bupa's food and symptoms diary (PDF, 1.4MB). Fill it out and take it with you to your GP appointment.
Helicobacter pylori (H. pylori) testing
If you’re having regular episodes of indigestion, your GP may suggest you have a test for H. pylori bacteria. H. pylori infection is a common cause of ulcers in your stomach or duodenum. You may have a breath test to check for H. pylori or your GP may recommend a poo (faecal) sample test instead.
Endoscopy
Depending on any other symptoms you have and your age, your GP may refer you for a test called an endoscopy (or gastroscopy). This involves a long flexible tube with a camera at the end so your doctor can see inside your oesophagus and stomach.
Your GP may refer you for this test if you’re finding it hard to swallow, or if you’re over 55 and are losing weight for no reason. Your GP may also suggest an endoscopy if your symptoms aren’t getting better with treatment.
GP Subscriptions – Access a GP whenever you need one for less than £20 per month
You can’t predict when you might want to see a GP, but you can be ready for when you do. Our GP subscriptions are available to anyone over 18 and give you peace of mind, with 15-minute appointments when it suits you at no extra cost.
Treatment of indigestion
You can usually treat mild indigestion yourself. Your pharmacist should be able to give you lifestyle advice, recommend suitable over-the-counter indigestion remedies, and suggest when to see your GP.
Lifestyle changes
There are several changes you can make that may help to stop indigestion or give you some relief.
- If you’re overweight, losing excess weight may help.
- Cut down on foods or drinks that may be triggering your symptoms – a food diary may help you keep track.
- Stop smoking , if you smoke.
- If you drink alcohol, make sure you’re drinking within recommended limits.
- Try to eat smaller meals at regular intervals during the day, rather than having one or two large meals.
- Sleep in a more upright position by raising the head of your bed with blocks of wood or bricks.
- Don’t eat during the three or four hours before you go to bed.
- Try and reduce any stress and anxiety.
Always tell your pharmacist or GP if you’re taking any medicines, as some medicines can cause indigestion or make it worse. Your pharmacist or GP will tell you if you should stop taking these medicines or change how you take them.
Indigestion medicines
You can buy several indigestion medicines over the counter without a prescription. Speak to your pharmacist about what’s most suitable for you. Your pharmacist will tell you if you need to see your GP. Your GP may be able to prescribe different medicines or longer courses.
Antacids
You can take antacids for occasional symptoms. These ease indigestion by neutralising acid in your stomach so it’s less likely to cause irritation. Antacids usually contain magnesium or aluminium. You can buy them from a pharmacy or shop, without a prescription from your doctor. You can take them when you have symptoms or if you’re expecting them to flare up (for example, before you go to bed).
Proton pump inhibitors
If antacids don’t work, or you need to take them regularly to ease your symptoms, your pharmacist may recommend a proton pump inhibitor. Proton pump inhibitors, such as omeprazole, are a type of medicine that work by stopping your stomach making acid. You can take an over-the-counter proton pump inhibitor without a prescription from your doctor for up to four weeks.
If you feel that you need to keep taking a proton pump inhibitor to control your symptoms, you should see your GP. They can assess you further and may prescribe a longer course. They’ll usually suggest you take a lower dose once your symptoms are under control.
Other medicines for indigestion
If you can’t take a proton pump inhibitor, you may be able to try histamine (H2) receptor antagonists, such as famotidine or nizatidine instead. These also work by reducing how much stomach acid you make.
If H. pylori bacterial infection is causing your indigestion, your GP may recommend a combination of medicines. You may need to take antibiotics to kill the bacteria, and proton pump inhibitors to reduce the amount of acid your stomach makes.
Always ask your GP or pharmacist if you have any questions about your medicine and read the patient information leaflet that comes with it.
Indigestion includes a range of symptoms affecting your upper abdomen. You might have a burning feeling or pain in your upper abdomen. Some people feel bloated, get full very quickly or feel sick. For more information, see our symptoms of indigestion section.
With indigestion, you tend to feel the pain in your upper abdomen, just under your ribs. Sometimes it might be higher up in your chest.
How long indigestion lasts depends on what’s causing it. It can often come and go. If you’re getting indigestion regularly and self-help measures aren’t working, you should see your GP.
Often, there’s no underlying reason for your indigestion. Your bowel might be particularly sensitive to acid, or certain foods may set off your symptoms. See your GP if you keep getting indigestion. Your GP will be able to check if there is any underlying condition causing your symptoms. For more information, see our causes of indigestion section.
Did our Indigestion information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Dyspepsia – unidentified cause. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2023
- Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management. National Institute for Health and Care Excellence (NICE). nice.org.uk, last updated October 2019
- Indigestion. Guts UK. gutscharity.org.uk, last accessed October 2023
- Assessment of dyspepsia. BMJ Best Practice. bestpractice.bmj.com, last reviewed 30 September 2023
- Dyspepsia – proven functional. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2018
- Dyspepsia – proven GORD. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last reviewed July 2023
- Dyspepsia – proven peptic ulcer. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2023
- Dyspepsia – pregnancy-associated. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2023
- Dyspepsia and gastro‑oesophageal reflux disease in adults. Quality standard. National Institute for Health and Care Excellence. nice.org.uk, published 23 July 2015
- Suspected cancer: recognition and referral. National Institute for Health and Care Excellence. nice.org.uk, last updated October 2023
- Heart attack. British Heart Foundation. bhf.org.uk, last updated March 2023
- Acute myocardial infarction (MI). MSD Manual. msdmanuals.com, last full review/revision June 2022
- Antacids. Patient. patient.info, last updated August 2023
- Omeprazole. NICE British National Formulary. bnf.nice.org.uk, last accessed October 2023
- H2 Blockers. Patient. patient.info, last updated July 2023



