Stroke
- Dr Ahamad Hassan, Consultant Neurologist and Stroke Physician
- Pippa Coulter, Freelance Health Editor
A stroke is when the blood supply to part of your brain is cut off. A stroke is a medical emergency. It's vital to recognise signs of a stroke quickly and get treatment in hospital as soon as possible.
About stroke
There are two main types of stroke.
- Ischaemic stroke. This happens when the blood supply to part of your brain is blocked. This might be by a blood clot or a clump of fatty material that blocks or narrows a blood vessel. It’s the most common type of stroke.
- Haemorrhagic stroke. This is caused by bleeding inside or around your brain. It can happen when a blood vessel bursts.
You can also have something called a transient ischaemic attack (TIA). This is also sometimes known as a ‘mini stroke’. This is when you have a blockage of blood to your brain, like an ischaemic stroke, but it’s only temporary. The symptoms last for less than 24 hours.
Strokes are a common reason for people being admitted to hospital in the UK. Strokes can be fatal, but more people are surviving them than ever before. For people who do survive a stroke, disability is common. Getting hospital treatment quickly can improve how well someone recovers after a stroke.
The risk of stroke increases as you get older. But anyone can have a stroke. And people are getting strokes at an earlier age than they used to. A third of strokes happen in people aged between 40 and 69.
Causes of stroke
A stroke is usually caused by a blood clot blocking a blood vessel, or a blood vessel bursting. This reduces or cuts off the blood supply to your brain, damaging your brain. You are at greater risk of stroke if you are male, as you get older, and if you have a family history of stroke.
There are also several medical conditions that can increase your risk of stroke. These include having:
- high blood pressure
- atrial fibrillation – a type of irregular heartbeat
- other conditions that affect your heart or how your blood clots
- high cholesterol
- diabetes
Certain lifestyle factors can increase your risk of heart and blood vessel problems. This can then make a stroke more likely. These can include:
- smoking
- being inactive (not doing much exercise)
- being overweight or obese
- having a poor diet
- drinking excessive amounts of alcohol
- using illegal drugs, such as cocaine
If you’ve already had a stroke or a TIA (‘mini stroke’), you’re at greater risk of having another one. There has also been research to show that having COVID can increase your risk of having a stroke. The risk is highest in the first few weeks following infection.
Symptoms of stroke
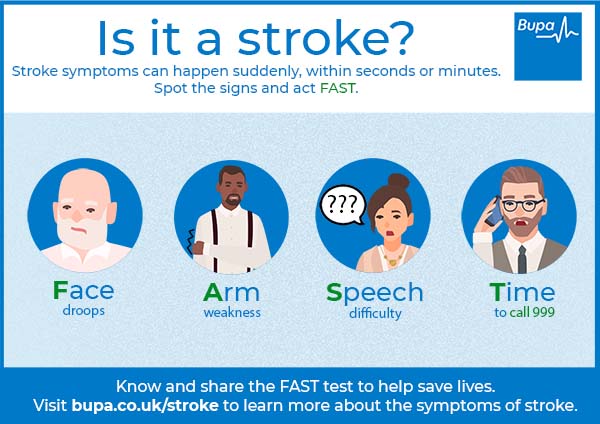
Stroke symptoms usually come on suddenly. A good way to recognise the signs of a stroke is to use the ‘FAST’ test.
- Face weakness. The person may not be able to smile. Their mouth or eye may also droop down on one side.
- Arms weakness. The person may not be able to raise their arms and hold them there.
- Speech difficulties. They may have slurred speech or find it difficult to remember the names of common objects.
- Time to call 999. If the affected person has one or more of these symptoms, call for emergency help straightaway.
Bupa's FAST test infographic (PDF, 0.5 MB), illustrates the signs of a stroke. Click on the FAST image below to download the PDF (0.5MB).
There can be other symptoms of stroke too. These can vary depending on the type of stroke and the part of the brain affected. But they can include:
- weakness, numbness or paralysis on one side of body, including in the legs, hands or feet
- blurred vision or loss of sight in one or both eyes
- feeling confused
- headache – this may come on gradually or be sudden and severe
- vertigo – you may feel as if things are spinning
- feeling sick or vomiting
Diagnosis of stroke
If you have a suspected stroke, you’ll be admitted to a specialist stroke unit to be assessed. Here, you will have a brain scan. This is to confirm whether or not you have had a stroke and if so, what type it is. There are two main types of scan you might have:
Your doctor may use a dye or ultrasound tests to help show up blood vessels that supply your brain. This can help to confirm what has caused your stroke, and what treatments may help.
When you’re in hospital, you are also likely to have some blood tests. These can rule out anything else that may have caused your symptoms. They can also check for possible causes of stroke. You may have tests of your heart too, including:
- an ECG (electrocardiogram), to check the electrical activity in your heart
- an echocardiogram – an ultrasound of your heart
Treatment of stroke
Your treatment will begin while you’re in hospital. You’ll be cared for by a team of doctors and nurses on a specialised stroke unit. If you’re having trouble breathing, you may have oxygen therapy via a face mask or a tube in your nose to help with your breathing. You may have fluid through a drip, and a feeding tube in your nose if you’re unable to swallow.
The exact treatment you have will depend on the type of stroke you’ve had and how severe it is.
Treatment of ischaemic stroke
If you’ve had an ischaemic stroke, your doctor might give you a medicine to dissolve any blood clot and restore blood flow to your brain. This will depend on how long it’s been since your stroke started, and the results of any scans.
Some people with ischaemic stroke may have a procedure called a thrombectomy to remove a blood clot. In this procedure, your doctor threads a tube (catheter) into a blood vessel in your groin, and through to where the clot is in your brain. They then insert a retrieval device to remove the clot. You may have this if the blood clot is in a large artery in your brain.
Some people who have had a very severe ischaemic stroke may need an operation to relieve pressure on the brain. This is called a decompressive hemicraniectomy. It involves opening up a section of the skull.
You’ll usually be offered aspirin or an alternative medicine after your stroke, to stop your blood clotting. You’ll also be offered ongoing treatments to help reduce your risk of having another stroke over the long term. These may include medicines to prevent your blood clotting, and to reduce your blood pressure and cholesterol level.
Treatment of haemorrhagic stroke
Sometimes haemorrhagic strokes can be a result of taking anticoagulant medicines. These are medicines that make your blood thinner and less likely to clot. If you take these and have had a stroke, your doctor will give you other medicines to reverse the effects of the anticoagulant. If you have high blood pressure, your doctor will give you medicines to lower it.
Sometimes, surgery can be an option for haemorrhagic stroke. Surgery can help to relieve a build-up of pressure in your skull, caused by the burst blood vessel. If your stroke is caused by a burst aneurysm (a bulge in a blood vessel), you may have surgery to repair it.
Some people have seizures after having a haemorrhagic stroke. If this happens, you may need to take anticonvulsants (medicines to prevent seizures).
Worried about your heart health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0800 665 577
Complications of stroke
How a stroke affects you is different for everyone. Some people recover from them quickly. Other people may have a range of ongoing problems. Some people don’t survive having a stroke.
Long-term complications can include the following.
- Physical problems. These may include weakness on one side of your body. You may have difficulties with co-ordination or balance, and stiff, tight muscles.
- Sensory problems. These include changes in how you feel touch, temperature and pain.
- Difficulty swallowing. This can make it hard to eat and drink.
- Feeling exhausted and having no energy.
- Pain. This might be due to damage caused by the stroke. Or, you might have muscle pain due to lack of movement following a stroke.
- Communication problems. These may include difficulties with your speech, reading and writing.
- Problems with your vision. You might have double vision, blurry vision or find it hard to see.
- Difficulties with thinking, memory, attention and concentration.
- Incontinence. This means difficulty controlling when you pee or poo.
- Emotional difficulties. Those close to you may notice changes in your behaviour or you may feel anxious or depressed.
- Sexual problems. These may be due to both the physical and emotional effects of your stroke.
- Related conditions, such as vascular dementia. This is a type of dementia caused by lack of blood supply to the brain. This can happen following a stroke.
These problems can make it difficult to carry on with your normal daily activities after having a stroke. You may find it a struggle to take care of yourself and to live independently.
Recovering from stroke
After you have recovered from the initial stroke, your care will be aimed at supporting your rehabilitation. This means trying to get back as close as possible to how you were before your stroke, or learn new ways of doing things.
Your rehabilitation may start in hospital. The doctors and nurses looking after you will assess you before you leave and work out a rehabilitation plan. Once you have left hospital, if you haven’t recovered, you should be seen by a specialist stroke rehabilitation team. Your GP can support you with getting the help you need. You may have support from a number of different health professionals, including:
- physiotherapists to help strengthen your muscles and improve your mobility, balance and coordination
- occupational therapists who can help you to re-learn everyday skills like dressing and caring for yourself
- speech and language therapists to help with any speech or swallowing difficulties
- a dietitian to make sure you’re getting all the nutrients you need
- counsellors or therapists, who can help provide emotional support
- a psychologist, to help with mood and memory problems
- an audiologist, who can check for hearing problems
- an orthoptist, to help with vision problems after a stroke
- continence nurses, for advice on exercises and treatments to help manage incontinence
Recovery and rehabilitation can take a long time. The health professionals you see will encourage you to set goals that you want to work towards. These are different for everyone. They might include things like becoming more mobile, or more independent. It can help you to focus on what you most want to achieve from rehabilitation.
When you’ve had a stroke, you are at increased risk of having another one. The greatest risk is in the first few days and weeks after the stroke. Around one in 10 people will have another stroke within a year, and four in 10 within 10 years. This will depend on many things though, like your age, other health conditions and lifestyle factors.
Part of your long-term treatment will be in trying to reduce your risk of having another stroke. Your GP should offer you regular reviews and advise you on things you can do to reduce your risk. We have more information on this in our prevention section.
Prevention of stroke
There are a number of things you can do to reduce your risk of having a stroke. This includes a first stroke, and if you’ve already had a stroke, your risk of having another. They include the following lifestyle measures.
- Being active every day, and reducing the time you spend sitting down.
- If you smoke, stopping smoking.
- Eating a healthy diet, with at least five portions of fruit and vegetables every day, and limiting saturated fat and salt.
- Maintaining a healthy weight, and losing excess weight if you need to.
- If you drink alcohol, making sure you don’t drink to excess.
It’s also important to take any medicines you’ve been prescribed for other conditions linked to stroke. These include high blood pressure, high cholesterol, diabetes and atrial fibrillation. Taking medicines to control these conditions will help reduce your risk of stroke.
The main types of stroke are ischaemic stroke and haemorrhagic stroke. An ischaemic stroke is when the blood supply to your brain is blocked by a blood clot or fatty material. A haemorrhagic stroke is due to bleeding in your brain. This is usually from a burst blood vessel. For more information, see our about stroke section.
Strokes are often caused by a blood clot or burst blood vessel in your brain. They can be linked to various medical conditions like high blood pressure and atrial fibrillation. Lifestyle factors like a poor diet and smoking can increase your risk. To find out more, see our section on causes of stroke.
A stroke can damage the brain and cause a number of long-term problems. These may include difficulties with movement, communication, vision and emotions. Someone who has had a stroke will be offered rehabilitation afterwards to help them recover. To find out more, see our section on recovery from stroke.
Exactly how much a stroke affects you will be very different for everyone. But fewer people survive haemorrhagic strokes than ischaemic strokes. Whichever type of stroke you have, it’s really important to seek medical help quickly. This will improve your chances of surviving the stroke. For more information, see our section on symptoms of stroke.
When you’ve had a stroke, your risk of having another one increases. Your own individual risk will depend on lots of things, including your age and other health conditions. But around one in 10 people who have had a stroke go on to have another within a year. The greatest risk is in the first few weeks after your stroke. Find out more in our section on recovery from stroke.
High blood pressure (hypertension)
Benefits of exercise
Not only does regular exercise help you manage your weight and reduce your risk of developing diseases, it can help prevent and treat mental health problems
How to start exercising
We should all be getting active – and it may be easier than you think. Here we give you tips and advice for getting started
Tips for a healthy and well-balanced diet
A healthy, well-balanced diet involves eating foods from a variety of food groups to get the nutrients that your body needs to function.
Effects of smoking
Tools and calculators
BMI calculator
BMI, or body mass index, is one way of measuring whether you’re a healthy weight for your height.
Simply enter your details into our calculator and the result will give you an indication of whether you're a healthy weight.
Calories calculator
If you want to lose weight, you need to increase your physical activity and watch your calorie intake. Bupa's calorie calculator will help you to work out how many calories you're burning in a day.
Other helpful websites
Discover other helpful health information websites.
Did our Stroke information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Stroke and TIA. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2023
- National Clinical Guideline for Stroke for the UK and Ireland. National Clinical Guideline for Stroke for the UK and Ireland. London: Intercollegiate Stroke Working Party; 2023 May 4. Available at: www.strokeguideline.org
- Ischaemic stroke. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 November 2023
- Stroke due to spontaneous intracerebral haemorrhage. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 November 2023
- Knight R, Walker V, Ip S, et al. CVD-COVID-UK/COVID-IMPACT Consortium and the Longitudinal Health and Wellbeing COVID-19 National Core Study. Association of COVID-19 with major arterial and venous thrombotic diseases: a population-wide cohort study of 48 million adults in England and Wales. Circulation 2022; 146(12):892–906. doi: 10.1161/CIRCULATIONAHA.122.060785
- Stroke and transient ischaemic attack in over 16s: diagnosis and initial management. National Institute for Health and Care Excellence (NICE), www.nice.org.uk, last updated 13 April 2022
- Stroke signs and symptoms. Stroke Association. www.stroke.org.uk, accessed 6 December 2023
- Mechanical clot retrieval for treating acute ischaemic stroke. Interventional procedures guidance IPG548. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 24 February 2016
- Ischaemic stroke. Stroke Association. www.stroke.org.uk, accessed 11 December 2023
- Haemorrhagic stroke. Stroke Association. www.stroke.org.uk, last accessed 11 December 2023
- Dementia. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised December 2022
- Next steps after a stroke. Stroke Association. www.stroke.org.uk, published December 2021
- Stroke rehabilitation in adults. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 18 October 2023
- Cardiovascular disease: risk assessment and reduction, including lipid modification. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 24 May 2023