Infrapatellar fat pad syndrome
Your health expert: Mr Damian McClelland, Trauma and Orthopaedic Consultant, and Clinical Director for Musculoskeletal Services at Bupa
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, July 2023
Next review due July 2026
Infrapatellar fat pad syndrome is a condition that causes knee pain. Your infrapatellar fat pad is one of three pads of fatty soft tissue that lie under your kneecap (patella), at the front of your knee. It’s also known as the Hoffa’s fat pad.
About infrapatellar fat pad syndrome
Your infrapatellar fat pad sits behind and just below your kneecap (patella), where it acts as a protective cushion, separating your kneecap from your shin and thigh bones.
Infrapatellar fat pad syndrome is when your fat pad becomes pinched (impinged) between your kneecap and thigh bone or between your thigh and shin bones. It’s also known as infrapatellar fat pad impingement and Hoffa pad impingement syndrome. Your infrapatellar fat pad has a rich supply of nerves, so impingement can be very painful.
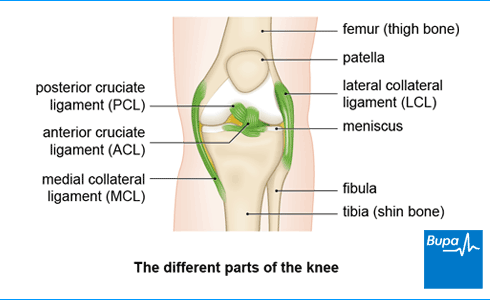
If you injure your infrapatellar fat pad, you may injure other parts of your knee at the same time – for example, your anterior cruciate ligament (ACL).
Causes of infrapatellar fat pad syndrome
Infrapatellar fat pad syndrome can be caused by a number of things. It can be caused by a sudden injury such as a direct blow to your knee. It can also be caused if you overextend your knee. This is when your knee is forced beyond its fully straightened normal position.
Infrapatellar fat pad syndrome can also develop gradually over time if you repeatedly overextend your knee.
Symptoms of infrapatellar fat pad syndrome
Infrapatellar fat pad syndrome can be extremely painful, like a burning or aching sensation. You’ll usually feel the pain at the front of your knee, around the bottom of your kneecap. This pain may be worse when:
- your leg is completely straight
- you stand for a long time
- you go up or down stairs
The area around the bottom of your kneecap may also feel very tender to the touch. You may have some swelling there too, and you may not be able to move your knee as well as usual.
Self-help for infrapatellar fat pad syndrome
It’s best to stop doing any activities that make the pain worse. This might mean:
- not standing for too long
- being aware not to over-extend your knee
- taking a break from doing any sports that usually make your pain worse
Treatment of infrapatellar fat pad syndrome
The initial treatment for infrapatellar fat pad syndrome aims to reduce pain and inflammation. You can try to do this with rest (see our section on self-help) and medicines. Further treatments include taping your knee and physiotherapy to gradually get you back to your usual activities. Your GP may be able to refer you to a sports medicine professional, such as a physiotherapist or a sports doctor. Or you can book an appointment with a physiotherapist yourself.
Infrapatellar fat pad syndrome will often get better with physical therapy and/or steroid injections (see below). For people who need an operation, most return to the level of sporting activity they had before they had infrapatellar fat pad syndrome.
Physiotherapy
Your physiotherapist will assess your knee and plan a programme of infrapatellar fat pad syndrome exercises to help strengthen your knee and leg muscles gradually. This may involve specific strengthening exercises and training in how to not overextend your knee. Make sure you do these exercises because they’re an important part of your recovery from infrapatellar fat pad syndrome.
Your physiotherapist may also recommend that you tape your knee. This is done in a particular way to relieve the impingement (pinching) on your fat pad. You may need to keep the tape on your knee until your pain has gone.
Medicines
Over-the-counter painkillers such as ibuprofen (a non-steroidal anti-inflammatory drug), may help to ease pain and reduce inflammation and swelling. Always read the patient information that comes with your medicine, and if you have questions ask a pharmacist for advice.
Your doctor may also offer you a corticosteroid injection into your knee joint to provide temporary pain relief.
Surgery
Most people with infrapatellar fat pad syndrome don’t need surgery. But if other treatments haven’t worked, it might be an option. There are different surgical procedures to treat infrapatellar fat pad syndrome. If your doctor recommends that you have surgery, they’ll discuss the risks and benefits of the operation with you.
Looking for physiotherapy?
You can access a range of treatments on a pay as you go basis, including physiotherapy.
To book or to make an enquiry, call us on 0370 218 6528∧
Infrapatellar fat pad syndrome will often get better with physical therapy. Sometimes, you may also need a steroid injection and it may go away after this treatment. Even if you need an operation, most people get better and return to the level of sporting activity they had before they had infrapatellar fat pad syndrome.
For more information, see our section on treatment of infrapatellar fat pad syndrome.
The main sign or symptom of infrapatellar fat pad syndrome is pain. It may feel like a burning or aching sensation, usually at the front of your knee, around the bottom of your kneecap. You may have some swelling on your kneecap too, and you may not be able to move your knee as well as usual.
For more information, see our section on symptoms of infrapatellar fat pad syndrome.
Infrapatellar fat pad syndrome can be caused by an injury. For example, you might have a direct blow to your knee or overextend your knee. Infrapatellar fat pad syndrome can also develop gradually over time if you repeatedly overextend your knee.
For more information, see our section on causes of infrapatellar fat pad syndrome.
You can treat infrapatellar fat pad syndrome with physiotherapy. Other treatments include taping your knee and steroid injections. If these treatments don’t work, you may need to have an operation but most people don’t need this.
For more information, see our section on treatment of infrapatellar fat pad syndrome.
Posterior cruciate ligament (PCL) injury
With a PCL injury, it’s common to injure other ligaments, or other parts of your knee, at the same time.
Anterior cruciate ligament (ACL) injury
An ACL injury can be a partial or a complete tear, an overstretch, or a detachment of the ligament.
Medial collateral ligament (MCL) injury
The MCL is the most commonly injured knee ligament. It often gets injured during sports such as rugby.
Meniscal tear
Tears of the menisci are a common injury. When people talk about a ‘torn cartilage’ in their knee they usually mean a meniscus injury.
Patellar tendinopathy (jumper's knee)
Patellar tendinopathy is also called ‘jumper’s knee’ because the injury commonly occurs during sports that involve jumping, such as basketball.
Patellofemoral pain syndrome
Patellofemoral pain syndrome is sometimes called ‘runner’s knee’ because it’s particularly common in people who run or do other sports.
Did our Infrapatellar fat pad syndrome information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Matthew Dubose. Hoffa pad impingement syndrome. StatPearls Publishing. www.statpearls.com, updated 22 February 2023
- Kuwabara A, Fredericson M. Narrative: Review of anterior knee pain differential diagnosis (other than patellofemoral pain). Curr Rev Musculoskelet Med 2021; 14(3):232–8. doi: 10.1007/s12178-021-09704-9
- Knee pain – assessment. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2022
- Find a physio. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 24 January 2023
- Treatment for knee pain. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 26 March 2020



