Bunion surgery
- Mr Jonathan Larholt, Consultant Podiatric Surgeon
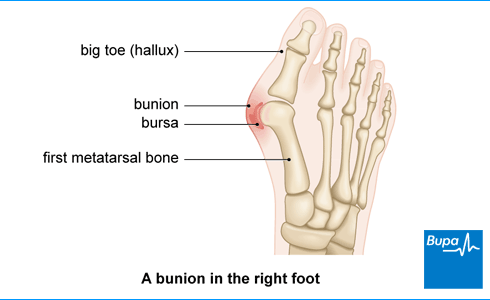
Bunion surgery is an operation to correct a bunion. A bunion is a deformity of your big toe joint. It causes a bony lump on the inside of your foot. This can be painful, especially when you’re walking or wearing shoes. Bunion surgery can remove or straighten the bone to ease your pain.
About bunion surgery
Bunions don’t always cause pain and discomfort. But they can get worse over time. Some bunions get worse more quickly than others. They may become very sore and make it harder for you to find shoes that fit properly. Bunion surgery may be recommended by your doctor if nothing else is easing your bunion pain. Surgery is sometimes also recommended if:
- you can’t buy well-fitting shoes
- you can’t walk properly
- the bunion is significantly affecting your daily life
Bunion surgery won’t be recommended just to make your foot look better.
Preparing for bunion surgery
Your surgeon will explain how to prepare for your operation. If you smoke, you should stop. This is because smoking makes you more likely to get a wound infection and slows down how quickly your bone heals. Bunion surgery is usually done as a day-case operation. This means you have the operation and go home on the same day. Sometimes your surgeon may recommend that you stay in hospital overnight. This might be because:
- you have another medical condition, such as diabetes or high blood pressure
- you’re in a lot of pain after the surgery
You may find it difficult to move around at first after surgery, especially if you’re using crutches. So, it’s a good idea to get your home ready before you go into hospital. You may need to rearrange furniture and other items so you can reach them easily. If your home has stairs, you may want to sleep downstairs if you can. You’ll need a friend or family member to stay with you for 24 hours after surgery.
You may have bunion surgery under local or general anaesthesia. With general anaesthesia you’ll be asleep during the operation. A local anaesthetic will be also used to numb your foot and reduce the amount of general anaesthetic that’s needed. If you decide to have a general anaesthetic, you’ll be advised when to stop eating and drinking.
If you have a local anaesthetic, you’ll stay awake during the operation. Your surgeon and anaesthetist will be able to advise on what’s best for your bunion surgery.
You may need to wear compression stockings to keep your blood flowing and to stop blood clots from forming in the veins in your legs. You may need to have an anti-clotting medicine as well.
Your surgeon will discuss with you what will happen before, during and after your surgery. If you’re unsure about anything, don’t be afraid to ask. No question is too small. It’s important that you feel fully informed so you’re happy to give your consent for the operation to go ahead. You’ll be asked to do this by signing a consent form.
What are the alternatives to bunion surgery?
If you have a bunion, your GP or podiatrist may recommend several other bunion treatments before opting for surgery. These include:
- taking over-the-counter painkillers such as paracetamol and ibuprofen to ease pain and swelling
- wearing bunion pads to ease pressure on the lump
- using ice packs to relieve the pain
- wearing insoles or orthotic supports in your shoes
- wearing splints at night to hold your toes straight
- wearing different shoes – for example, low-heeled, wide-fitting shoes that are soft enough to fit around the bunion
Bunions often get worse over time. So, if the above measures aren’t helping and you’re in a lot of pain, your GP may refer you for surgery.
What happens during bunion surgery?
Surgery to remove a bunion usually takes about an hour. But the timing depends on which operation you’re having. There are over 100 different types of bunion surgery. Your surgeon will discuss which one is best for you. This will depend on many things, including:
- the size of your bunion
- what you do for work and socially
- your overall health
The most common type of bunion removal surgery is called a metatarsal osteotomy. This involves cutting away the bunion and re-aligning the bones of the joint to make the side of your foot straighter. Your surgeon may make a cut over your big toe joint to remove the bunion. Or they may do keyhole bunion surgery, reaching the bunion through several smaller cuts.
Once the bunion has been removed, your surgeon may use screws or staples to hold everything in place. These are usually left in place permanently but can be removed later if necessary.
If you have bunions on both feet, it’s possible to have surgery to treat these at the same time. But this isn’t usually recommended because you won’t be able to walk on either foot afterwards. Your surgeon will be able to discuss whether or not this may be an option for you.
How bunion removal surgery is carried out
What are bunions | The procedure | Watch in 1 minute 35
A bunion is a lump of bone on the knuckle of your big toe. They can cause pain and discomfort. This video shows one type of bunion removal surgery, and what happens during the operation.
The video contains an animation will show how a bunion can be treated using surgery.
A bunion is a lump of bone on the knuckle of your big toe.
The bone of the big toe won't be aligned as it should be.
A bunion can cause discomfort, pain, swelling and redness in and around the big toe.
If left untreated, it can make walking difficult.
There are lots of different operations to treat a bunion.
This animation shows one type of metatarsal osteotomy operation.
You will be given a general anaesthetic.
This means you will be asleep during the operation and feel no pain.
Cuts will be made in the foot.
Your surgeon will remove the part of the bone that is protruding.
The first metatarsal bone will also be cut and repositioned to help straighten the foot.
Your surgeon may also reposition the ligaments and tendons within your foot.
The bone is fixed into place with screws, wire or staples while your foot heals.
The cuts are closed with stitches and a dressing is placed over your foot.
This is the end of the animation.
What to expect afterwards
You’ll need to rest until the effects of the anaesthetic have worn off. You may need to take some medicines to relieve pain. Your foot will probably be in a bandage after the operation. Your hospital will usually give you some crutches and a special shoe to wear. They’ll also advise you how much (if any) weight you can put on your foot.
A physiotherapist may visit you after your operation to show you how to move around without hurting yourself. They can also teach you how to use crutches and arrange another appointment if you need more help.
You’ll be able to go home when you feel ready, and the surgeon considers it safe. This may be about an hour or two after your operation. Your nurse may give you a date for a follow-up appointment before you leave.
Everyone reacts differently to having a general anaesthetic. If you’ve had one, you may feel particularly tired afterwards. You may also find that you’re not so co-ordinated or it’s difficult to think clearly. This should pass within around 24 hours. In the meantime, don’t drive, drink alcohol, operate machinery or sign any important documents.
Recovering from bunion surgery
After your operation, you’ll be given painkillers. Always read the patient information leaflet that comes with your medicines. If you have any questions, ask your pharmacist for advice. You may have some pain in the first 24 to 48 hours, then it will improve.
If you continue to have pain after 48 hours, contact your surgeon. Keep your dressing dry. Your surgeon will give you advice on washing and bathing after your operation. Your surgeon will give you specific advice. But you’ll probably be able to put weight on your other foot (the one that didn’t have the surgery) straight away.
It’s important to rest with your foot up for the first couple of weeks because this will help to reduce any swelling.
You’ll usually have dressings and a bandage on your foot after bunion surgery. You may also need to wear a surgical (post-operative) shoe, a cast, or a boot. Your surgeon will advise how long to wear it for.
You may need to use crutches for up to six weeks after surgery. Your surgeon or physiotherapist will advise you on exercises for your foot, ankle, and big toe joint. It usually takes three to six months to get back to normal walking or sports activities after bunion surgery. But everyone recovers differently.
Bunion surgery recovery time can take up to a year. The main thing is to not do too much, too soon.
You can usually drive again once you’re able to do an emergency stop safely. But check with your surgeon and car insurance company first. You’ll also need to wait until you’re able to wear normal shoes again – this may take six to eight weeks.
How quickly you can return to work will depend on your job. If your job involves sitting down most of the time, you can probably go back to work six weeks after bunion surgery.
But if your job involves a lot of standing, walking, carrying or lifting, you may need to be off work for up to 12 weeks. Whether or not you drive to work will also affect when you can return to work. Your surgeon or specialist nurse will be able to advise you on this.
Side-effects of bunion surgery
Side-effects after bunion surgery include:
- a sore foot, especially your big toe
- swelling of your foot
It may take six months to a year for your swelling to go down completely.
Complications of bunion surgery
Bunion surgery can cause some complications. These include:
- a stiff toe – this doesn’t bother most people, but it can be important for athletes or dancers
- a numb toe – the nerves in your toe may be injured
- an abnormal toe position – your big toe may heal out of line and bend outwards or upwards; it may be slightly shorter
- an infection – for which you may need antibiotics
- pain under the ball of your foot – this can happen if there’s a change in the distribution of your weight
- the bunion coming back – or a corrected bunion may get worse so you may need to have another operation
When to see or contact your doctor
Contact your hospital or GP if you have:
- a high temperature
- worsening pain or pain that doesn't get better when you take painkillers
- redness around your dressing or if it feels warm
- swelling or pain in your calf muscle of your leg
- any discharge from your wound
Physiotherapy services
Our evidence-based physiotherapy services are designed to address a wide range of musculoskeletal conditions, promote recovery, and enhance overall quality of life. Our physiotherapists are specialised in treating orthopaedic, rheumatological, musculoskeletal conditions and sports-related injury by using tools including education and advice, pain management strategies, exercise therapy and manual therapy techniques.
To book or to make an enquiry, call us on 0345 850 8399
Not everyone needs bunion surgery. You may be able to ease your symptoms with self-help measures such as bunion pads and painkillers. But bunions can get bigger and hurt more over time. If you’re in a lot of pain or can’t wear shoes, you may need to have surgery.
For more information, see our section on the alternatives to bunion surgery.
You may be able to wear high-heeled shoes occasionally if your foot recovers well after bunion surgery. But you’ll need to wear more comfortable shoes such as trainers and flat boots for the first few months. Your podiatrist can give you advice about good foot care and how to prevent getting a bunion in the future.
You won’t be able to walk straightaway. You’ll need to rest the foot that’s been operated on for a couple of weeks. You may then need to walk with crutches for the first six weeks. You may also need to wear a special shoe, cast or boot.
For more information, see our section on recovering from bunion surgery.
Your foot may be painful following the surgery. You’ll be given painkillers while you’re in hospital and to take home with you. Contact your surgeon if your pain isn’t getting any better or is getting worse after 48 hours.
General anaesthesia
General anaesthesia is when medication is given to make you temporarily unconscious during an operation, so don't feel pain or other sensations.
Local anaesthesia
Local anaesthesia involves numbing a small part of your body with a medicine called a local anaesthetic to stop pain during and after surgery.
Over-the-counter painkillers
Bunions
A bunion is a painful lump that can develop on the side of your foot and affect how you walk.
Did our Bunion surgery information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Minimally invasive percutaneous surgical techniques with internal fixation for correcting hallux valgus. NICE Interventional procedures guidance IPG789. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published June 2024
- Hallux valgus. Patient. patient.info, last updated December 2022
- Bunion. MSD Manuals. msdmanuals.com, reviewed/revised November 2023
- A Guide to Bunion Surgery. British Orthopaedic Foot & Ankle Society. www.bofas.org.uk, accessed July 2024
- Preparing for surgery. Fitter. Better. Sooner. Royal College of Anaesthetists. www.rcoa.ac.uk, published May 2022
- Patient FAQs. Royal College of Anaesthetists. www.rcoa.ac.uk, published June 2019
- Caring for someone recovering from the general anaesthetic or sedation. Royal College of Anaesthetists. www.rcoa.ac.uk, published November 2021
- You and your anaesthetic. Royal College of Anaesthetists. www.rcoa.ac.uk, published April 2023
- Peripheral nerve blocks. Royal College of Anaesthetists. www.rcoa.ac.uk, published April 2023
- Prevention of deep vein thrombosis. Patient. patient.info, last updated June 2023
- Good surgical practice. Consent. The Royal College of Surgeons, www.rcseng.ac.uk, accessed July 2024
- Bunions (hallux valgus). Royal College of Podiatry. rcpod.org.uk, accessed July 2024
- Bunion. Medscape. emedicine.medscape.com, updated September 2023
- Bunions. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2021
- Common postoperative complications. Patient. patient.info, last updated November 2023
- Robinson C, Bhosale A, Pillai A. Footwear modification following hallux valgus surgery: The all-or-none phenomenon. World J Methodol 2016; 6(2):171–80. Published June 2016
- Personal communication by Mr Jonathan Larholt, Consultant Podiatric Surgeon, August 2024
- Victoria Goldman, Freelance Health Editor



