Bunions
Your health expert: Mr Jonathan Larholt, Podiatric Surgeon
Content editor review by Rachael Mayfield-Blake, January 2023
Next review due January 2026
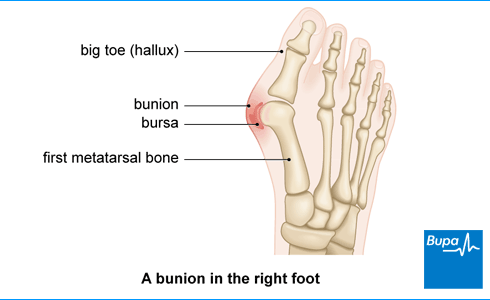
A bunion is a bony lump on the side of your foot at the base of your big toe. It can develop when your big toe leans in towards your other toes. A bunion can rub against your shoe and become sore, especially when you walk.
What is a bunion?
A bunion (hallux valgus) affects the front of your foot, on your big toe. You may first notice that you have a bunion when your big toe starts to bend towards your second toe. The bone at the base of the big toe gets pushed to the side and sticks out. This causes the bunion, which can be painful and may affect the way you walk (also called your gait).
Bunions are the most common problem that affects the front part of the foot in adults.
Causes of bunions
Doctors don’t know exactly what causes bunions, but some things can increase your risk of developing one.
- If your shoes don’t fit well and are too small or too tight, or you frequently wear high heels, it may increase your chance of getting a bunion.
- Bunions can run in families.
- If you’re ‘flat-footed’ and the arches of your feet are flatter than they should be because your arches have dropped, you’re more likely to get a bunion.
- If your foot rolls inwards when you walk, it can cause a bunion to form.
- If you have a long-term condition that affects your joints – for example, rheumatoid arthritis or gout – you may be more likely to develop a bunion.
- Anything that affects how you walk – for example, a foot injury, stroke or multiple sclerosis can make you more likely to have a bunion.
- Bunions are more common in women.
- Getting older increases your risk of developing a bunion because of the way age affects your joint movement.
Symptoms of bunions
Some people don’t get any symptoms from bunions. But if you do get bunion symptoms, they may include:
- a red or swollen big toe
- pain in the joints of your toes, especially when you walk
- pain in your foot – for example, under the ball of your foot
Your bunion may get bigger and feel more painful over time. You may find it harder to walk due to the pain. A bunion can also affect your balance and increase your chances of a fall. It may be hard to find comfortable shoes.
Sometimes, the skin over your bunion can get red, blistered or infected because it rubs against your shoe. A fluid-filled space called a bursa may form under your skin. This can be painful if it swells up (this is called bursitis).
If you have any of these symptoms of a bunion, see your GP. They may be able to refer you to a podiatrist (a healthcare professional who specialises in foot conditions). Alternatively, you can see a podiatrist privately. These symptoms can be caused by problems other than bunions, so it’s important to get them checked out.
Diagnosis of bunions
The GP or podiatrist will diagnose your bunion by asking about your symptoms. They’ll also examine your feet and may ask you to walk around so they can see how the bunion affects the way you walk.
You may need to have blood tests to rule out other health conditions – for example, rheumatoid arthritis or gout.
If you need to have bunion surgery, you may have further tests such as an X-ray.
Self-help for bunions
There are ways to ease the symptoms of bunions.
Footwear
One of the most important things you can do if you have a bunion, is to wear the right footwear. Try to resist any temptation to wear high heels. Instead, wear shoes with a low heel, a wide front and a thick, soft sole. Make sure your shoes have a back strap support because backless shoes force your toes to claw as you walk. Over time, this can strain your muscles.
Padding and splints
If you put a bunion pad over the bony lump, it may protect your feet from the pressure of your shoes. You can buy these pads from a pharmacy or from a podiatrist.
There are splints that you can wear at night to ease the pain from a bunion.
Shoe inserts
A podiatrist may recommend shoe inserts (orthoses or orthotics), which can be designed specifically for your foot.
Ice
If your bunion is painful and swollen, you can put something frozen on it. A bag of frozen peas is ideal but don’t leave it on any longer than 10 minutes at a time. And don’t put ice directly onto your skin because ice can damage skin – wrap the ice in a towel first. If you have diabetes or poor blood flow to your feet, speak to a GP or podiatrist first.
Exercises
Weak muscles in your foot and leg may affect bunion-related pain and movement problems. There are exercises you can do each day that may strengthen your muscles and ease the symptoms of bunions. There isn’t any evidence to prove these exercises work but if you decide to try them, it may help to combine them with other self-help methods. More research is needed to know for sure.
Do all these exercises barefoot and hold each stretch for 5 seconds. Keep going until you feel the muscles getting tired. You can start doing them sitting down in a chair before you progress to standing up and eventually balancing on one leg.
- Try to shorten your foot while you keep your heel and the front of your foot on the ground but don’t curl your toes.
- Lift and spread your toes while you keep your heel and the front of your foot on the ground. While your toes are spread out, push your little toe down and out. Then push your big toe down toward the inside of your foot.
- Stand with your knees bent then raise your arch while you keep your heel turned in. Then raise your heel off the floor while you keep pressure on your big toe.
Treatment of bunions
The self-help measures above will help ease the symptoms of a bunion but they won’t stop your bunion from getting worse over time. If your bunion causes severe pain, only an operation can correct it.
Medicines
You can take over-the-counter painkillers such as paracetamol or ibuprofen to help ease any pain and swelling caused by a bunion. Always read the patient information leaflet that comes with your medicine. If you have any questions, ask a pharmacist for advice.
If your bunion is caused by arthritis, a GP may recommend you have a steroid injection into your toe joint. This may also be an option if you don’t have arthritis but your bunion is red and swollen (inflamed).
Surgery
If you’ve tried self-help measures and medicines but they haven’t helped, bunion surgery may be necessary. A GP may refer you to an orthopaedic or a podiatric surgeon to see if this is an option for you. A GP can only refer you for bunion surgery under the NHS if:
- your bunion is very painful and is getting worse
- your second toe is also affected by the bunion
- you’re struggling to find any shoes that fit
- the bunion is badly affecting your day-to-day life
- you still have symptoms after trying self-help measures, shoe modifications and medicines for three months
If you want to have surgery because of how your bunion looks, you’ll need to have private treatment. Surgery isn’t recommended just to make your foot look better because it can cause complications.
There are lots of different types of bunion surgery. Simple surgery will reduce the lump on your foot, while more complicated surgery may also make your big toe as straight as possible. The best type of surgery for you will depend on how bad your bunion is, your lifestyle and if you have arthritis.
An operation won’t return your foot to normal but it may help to ease your symptoms and improve the shape of your foot. You may need to wear shoe inserts after your operation to reduce your chances of getting a bunion again.
Physiotherapy services
Our evidence-based physiotherapy services are designed to address a wide range of musculoskeletal conditions, promote recovery, and enhance overall quality of life. Our physiotherapists are specialised in treating orthopaedic, rheumatological, musculoskeletal conditions and sports-related injury by using tools including education and advice, pain management strategies, exercise therapy and manual therapy techniques.
To book or to make an enquiry, call us on 0345 850 8399
Prevention of bunions
You can help to prevent getting a bunion by wearing the right type of footwear. Ask a podiatrist for advice. They’ll probably recommend that your footwear:
- is wide enough, so there isn’t any pressure on the joints at the sides of your feet and you can wiggle your toes comfortably
- has a heel lower than four centimetres so your feet aren’t pushed forwards (if you wear high heels, vary your heel heights from day to day – wear higher heels one day and lower heels the next day)
- has adjustable fastenings such as laces, buckles or straps that hold your feet comfortably inside your shoe or boot
- has a back strap support because backless shoes force your toes to claw as you walk, which can strain your muscles over time
They may also suggest you use shoe inserts (orthotics or orthoses) to correct your walking if you have problems.
A bunion won’t cause osteoarthritis in your big toe but your big toe joint is more prone to osteoarthritis than any other joint in your foot. This is because of the repeated pressure you put on it when you walk. If you already have osteoarthritis in your big toe, you may be more likely to get a bunion. This is because the damaged cartilage can make your big toe lean towards your other toes.
How long it will take to walk after bunion surgery will depend on which operation you’ve had and how you recover. You may be able to walk around a bit the day after your operation. You might need to wear a modified shoe to protect your foot as you recover. You may also need to use some support to help you walk – for example, crutches. It can take up to a year to recover fully.
You can get a bunion on your little toe but this is much less common than a bunion on your big toe. A bunion on your little toe is called a bunionette or a tailor’s bunion. It’s treated in the same way as a bunion on your big toe.
There isn’t one main cause of bunions but several things that can increase your risk of developing one. These include wearing high heels, and being ‘flat-footed’. Bunions can run in families too. And you may be more likely to get a bunion if you have a long-term condition that affects your joints – for example, rheumatoid arthritis or gout.
For more information, see our section on the causes of bunions.
There are lots of ways you can ease the symptoms of a bunion without surgery. These include things like using padding to protect your feet and using shoe inserts. You can also take painkillers to ease pain and swelling from a bunion. But these measures won’t ‘fix’ your bunion. Only surgery can do this.
For more information, see our sections on self-help for bunions and treatment of bunions.
There are exercises you can do each day that may strengthen your muscles and help ease pain and problems walking due to bunions. More research is needed to prove whether or not such exercises help. If you do try the exercises, you can start doing them sitting down in a chair until you’re able to do them standing up and eventually balancing on one leg.
For more information, see our section on self-help for bunions.
Bunion surgery
Bunion surgery is an operation to remove or realign the bone that sticks out on your big toe when you have a bunion.
Osteoporosis
Over-the-counter painkillers
Physiotherapy
Gout
A condition that causes sudden swelling and severe pain in your joints.
Did our Bunions information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Bunions. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2021
- Bunions (hallux valgus). Royal College of Podiatry. rcpod.org.uk, accessed 13 January 2023
- Hallux valgus bunions. Patient. patient.info, last edited 13 December 2022
- Pes planus (flat feet). Patient. patient.info, last edited 14 January 2022
- A guide to bunion surgery. British Orthopaedic Foot and Ankle Society. www.bofas.org.uk, accessed 13 January 2023
- Bunion. MSD Manuals. msdmanuals.com, last full review/revision October 2021
- Bunion. Medscape. emedicine.medscape.com, updated 21 May 2021
- Bunion: Strengthening foot muscles to reduce pain and improve mobility. J Orthop Sports Phys Ther 2016; 46(7):606. doi:10.2519/jospt.2016.0504
- Ying J, Xu Y, István B, et al. Adjusted indirect and mixed comparisons of conservative treatments for hallux valgus: A systematic review and network meta-analysis. Int J Environ Res Public Health Apr 2021; 18(7):3841. doi: 10.3390/ijerph18073841
- Hallux valgus. British Orthopaedic Foot and Ankle Society. www.bofas.org.uk, accessed 13 January 2023
- Osteoarthritis. Royal College of Podiatry. rcpod.org.uk, accessed 16 January 2023
- Bunionette (tailor's bunion). Medscape. emedicine.medscape.com, updated 31 March 2022



