Chronic kidney disease
- Dr Richard Hull, Consultant in Renal Medicine
Chronic kidney disease (CKD) is when your kidneys don’t work as well as they should. It’s often caused by health issues like diabetes or high blood pressure. CKD is usually mild, but for some people, it can get worse over time. There’s no cure, but early treatment can help slow it down.
About chronic kidney disease (CKD)
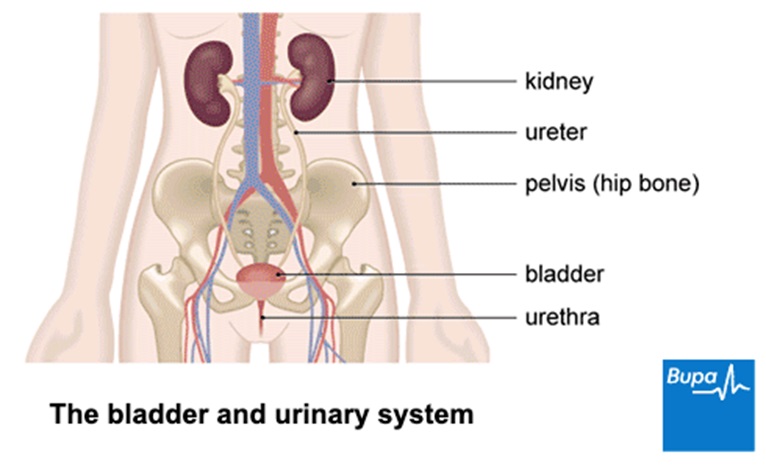
Most people have two kidneys. They’re shaped like beans and located in your lower back – one on either side of your spine. Your kidneys have lots of important jobs. They filter waste products and excess water from your blood and get rid of them in your pee (urine). They also help to make red blood cells, regulate your blood pressure, and keep your body’s fluids under control. But if your kidneys become damaged, these waste products can build up in your body and lead to problems with your health.
In medical terms, the word chronic tends to mean something lasts for a long time and gradually gets worse. If you’re diagnosed with chronic kidney disease (CKD), it means your kidneys haven’t been working properly, or there’s been too much protein in your pee , for at least three months. For more information on this, see our diagnosis section below.
CKD can affect anyone. Almost 1 in 10 people have the condition. But you’re more likely to develop kidney issues as you get older, or if you have diabetes or high blood pressure . It’s also more common in Black or Asian communities.
Chronic kidney disease stages
If you’re diagnosed with chronic kidney disease (CKD), your doctor will let you know what stage of CKD you have. They’ll use the results of blood and urine (pee) tests to figure this out. There are five CKD stages, depending on whether your condition is mild, moderate, or severe. At stage one, your kidneys are still working properly and you don’t have kidney disease. But tests might show other early signs of kidney damage. At this point, your doctor will help you manage any underlying health conditions and suggest lifestyle changes to try and stop kidney disease from developing later on.
But kidney disease can get worse over time and may eventually lead to stage five kidney failure. This means your kidneys have stopped, or almost stopped, working completely and you’ll need life-saving treatment called dialysis, or a kidney transplant. If there’s a chance this could happen, you’ll be referred to a kidney specialist called a nephrologist for support.
Chronic kidney disease causes
Chronic kidney disease (CKD) often develops if you have another health condition that damages your kidneys. CKD can be caused by the following.
- Diabetes. High blood sugar can slowly damage the tiny filters (called glomeruli) inside your kidneys.
- High blood pressure. Too much pressure on the blood vessels inside your kidneys can impact how well they work.
- Glomerulonephritis. This is an inflammation of the filters inside your kidneys, which can damage them.
- Some medications. Regular use of drugs like non-steroidal anti-inflammatories (NSAIDs) or lithium can harm your kidneys over time.
- Polycystic kidney disease. This genetic condition causes fluid-filled cysts to grow inside your kidneys and reduce how well they work.
- A blocked urinary tract. Blockages like kidney stones or an enlarged prostate can damage your kidneys by slowing or stopping the flow of pee (urine).
- Abnormal kidney structure. Being born with unusually shaped or sized kidneys increases your chance of developing CKD.
- Family history. Having a biological family history of CKD also increases your likelihood of developing it.
- History of kidney problems. You’re more likely to develop CKD if you previously had a sudden decline in kidney function, for example from a severe illness. This is known as an acute kidney injury.
Chronic kidney disease symptoms
You might not know that you have chronic kidney disease (CKD) at first, because it doesn’t always cause symptoms in the early stages. CKD is often discovered during a routine blood or urine (pee) test for something else.
But if your CKD has developed into severe kidney disease or kidney failure, symptoms may include:
- feeling sick or being sick
- blood in your pee (urine)
- peeing more or less often than usual
- peeing at night
- losing your appetite and losing weight
- swelling in your hands, feet, or ankles
- muscle cramps, which may be worse at night
- feeling tired and weak
- itchy skin
- trouble sleeping
- difficulty concentrating
- feeling out of breath
- a bad smell or taste in your mouth
- aching in your bones
- pale skin or a skin rash
- restless legs syndrome
Speak to your doctor if you have any of these symptoms. Finding and treating CKD early improves your chances of slowing it down.
Chronic kidney disease diagnosis
Chronic kidney disease (CKD) is often caused by other health conditions. So if you’re at a high risk for kidney issues, your doctor will invite you for regular check-ups. High-risk factors include high blood pressure, diabetes, heart disease, or a family history of CKD. These check-ups help monitor how well your kidneys are working and find CKD early.
CKD is usually diagnosed with blood and urine (pee) tests. But your doctor might recommend you have several tests to figure out if you have CKD, what could be causing it, and what stage it’s at. These could include the following.
Blood tests
Your doctor will take a sample of your blood and send it off to a lab for testing. They’ll check the levels of important vitamins and minerals, as well as how much creatinine is in your blood. Creatinine is a waste product produced by your muscles as they break down energy. Normally, your kidneys filter creatinine out of your blood and it leaves your body through urine (pee). But if your kidneys aren’t working properly, creatinine builds up in your blood.
Your doctor will use your creatinine result to estimate the glomerular filtration rate (GFR) of your blood. Glomeruli are tiny filters inside your kidneys. This is a measure of how much fluid your kidneys filter. A low GFR is a sign your kidneys might not be working as well as they should, and doctors use this to determine the stage of CKD.
Urine tests
Your doctor will also ask you to provide a urine (pee) sample for testing. They’ll check the albumin-to-creatinine ratio (ACR) of your pee. Albumin is a protein that’s usually found in your blood. But if albumin leaks into your pee, it indicates kidney damage. Knowing the albumin-to-creatinine ratio (ACR) helps your doctor to assess just how much protein is leaking into your urine and monitor your kidney health over time.
Imaging tests
Your doctor might recommend you have an ultrasound, CT scan, MRI scan or X-ray so they can get a better look at the size, shape, and structure of your kidneys. This will help your doctor to see if there’s anything blocking your kidneys, like a cyst, kidney stone, tumour or other structural problem.
Kidney biopsy
Sometimes, your doctor might want to take a tiny sample of tissue from your kidney to examine it more closely under a microscope. This helps them to get a closer look at the damage inside your kidney, so they can find out how far advanced it is and plan your treatment. During the biopsy, a fine needle is used to remove the tissue and you’ll be given a local anaesthetic to numb the area.
Self-help for chronic kidney disease
Although you can’t reverse kidney damage, there are lots of things you can do to live well with chronic kidney disease (CKD) and help prevent it from getting worse. It’s a good idea to make some lifestyle changes to help your kidneys work at their best, such as:
- eating less than 6g of salt a day
- limiting your alcohol intake to no more than 14 units a week
- keeping as active as you can
- maintaining a healthy weight
- stopping smoking , if you smoke
- taking any medication prescribed by your doctor
- keeping your annual vaccinations up-to-date
- attending regular check-ups with your healthcare team
- not taking dietary supplements like creatine
- avoiding taking non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, unless your doctor has prescribed them
Chronic kidney disease treatment
The type of treatment you’ll need for chronic kidney disease (CKD) will depend on the stage of your CKD. Treatment aims to help you live well, slow down the progression of CKD and keep your kidneys working well for as long as possible.
Medication
Medications can help to treat the underlying cause of your CKD and help prevent further complications from developing. Depending on what’s causing your CKD, your doctor might recommend you take:
- ACE (angiotensin converting enzyme) inhibitors or ARB (angiotensin receptor blockers) to lower your blood pressure
- statins or antiplatelets to lower your risk of heart disease or stroke
- SGLT-2 inhibitors (sodium–glucose cotransporter inhibitors) to keep diabetes and ACR levels under control
- diuretics to help you pee more and reduce swelling
- hormone injections or tablets that help your body make red blood cells if you have anaemia
- supplements to maintain a healthy level of vitamins and minerals in your body
Dialysis
If you have severe, end-stage kidney disease or kidney failure, you’ll need to have dialysis or a kidney transplant. Dialysis is a treatment that works like an artificial kidney to remove waste and excess water from your blood. There are two types of dialysis.
- Haemodialysis. This is when a machine filters your blood outside your body. Blood flows through a tube to the machine, which removes waste and extra fluid before returning clean blood to your body. It’s usually done three times a week for about four hours, though you can choose to have it more often. You can have haemodialysis done at home or in hospital.
- Peritoneal dialysis. This type of dialysis uses your peritoneum – the thin lining on the inside of your tummy – as a filter. A cleansing fluid is passed into your tummy using a tube. The fluid absorbs waste from inside your body and is then drained out. You can have peritoneal dialysis at home and you or a relative or carer can be trained to do it. But it must be done several times a day manually, or with a machine at night while you sleep.
Kidney transplant
If you have end-stage kidney disease, a kidney transplant may be another option. This involves placing a healthy kidney from a donor into your body. But a transplant is major surgery and isn’t suitable for everyone. So, your healthcare team will assess if you’re eligible for one first.
If you’re approved, you’ll usually be put on the waitlist for a kidney to become available from someone who has died. Or sometimes, a living relative, friend, or even stranger might choose to donate their kidney to you. Not only can a kidney transplant be life-saving, but it can also improve the quality of your life because you might not need dialysis anymore.
After a kidney transplant, you’ll need to take medicines called immunosuppressants to stop your body rejecting the kidney and go for regular check-ups for the rest of your life.
If you choose not to have dialysis or a transplant, or you’re not a suitable candidate, your healthcare team will help manage your symptoms. They’ll also focus on keeping you as comfortable as possible.
Chronic kidney disease complications
Over time, chronic kidney disease (CKD) can lead to other health problems. But finding and treating kidney issues as early as possible can reduce the chances of this happening. The main complications of CKD include:
- heart disease, stroke and other conditions that affect your heart and blood vessels
- high blood pressure
- high potassium levels (hyperkalaemia)
- a low red blood cell count (anaemia), which might make you feel tired
- a build-up of fluid that causes swelling around your legs, feet, and hands
- too much acid in your blood (acidosis)
- an imbalance in vitamins and minerals, which makes your bones weaker
Chronic kidney disease prevention
If you have an existing health condition that could lead to chronic kidney disease (CKD), managing this well will reduce your chance of developing CKD. This could include:
- attending regular check-ups with your doctor
- taking any medication you’ve been prescribed
- making healthy lifestyle changes to keep diabetes or high blood pressure under control
Leading a healthy lifestyle can also help to keep your kidneys working well. Aim to:
- maintain a healthy weight
- eat a nutritious, balanced diet
- do at least 150 minutes of moderate exercise a week
- limit your alcohol intake to 14 units or less over the week
- eat no more than 6g of salt a day
- drink plenty of fluids to stay hydrated
- stop smoking, if you smoke
- avoid taking NSAIDs, like ibuprofen, regularly unless advised by your doctor
GP Subscriptions – Access a GP whenever you need one for less than £20 per month
You can’t predict when you might want to see a GP, but you can be ready for when you do. Our GP subscriptions are available to anyone over 18 and give you peace of mind, with 15-minute appointments when it suits you at no extra cost.
Chronic kidney disease (CKD) often develops when an existing health condition damages your kidneys. The most common causes are diabetes and high blood pressure. But there are lots of other things that can also increase your risk. For more details, see our causes section.
Chronic kidney disease (CKD) doesn’t usually cause symptoms in the early stages. But advanced kidney disease can make you feel tired, sick, and need to pee more often. It can also cause swelling in your hands, feet, or ankles. See our section on symptoms for more information.
Chronic kidney disease (CKD) can’t be cured or reversed. But finding and treating it early can help stop it getting worse and prevent complications. This is why regular check-ups are essential if you have a health condition that raises your risk of CKD.
The treatment for chronic kidney disease (CKD) depends on what stage of CKD you have. In the early stages, you might need medication to treat the underlying cause and prevent further complications. But if your kidney disease is severe, dialysis or a transplant may be necessary. See our treatment section for more information.
High blood pressure (hypertension)
Managing type 2 diabetes
A few lifestyle tweaks here and there can help you keep your blood sugar steady and reduce your risk of complications.
High cholesterol
Cholesterol is a type of fat (lipid) made by your body and found in some foods.
Microalbuminuria
Microalbuminuria means that there’s more of a protein called albumin leaking from your kidneys into your urine than normal
Other helpful websites
- Kidney Care UK
Discover other helpful health information websites.
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Chronic kidney disease. Patient. patient.info/doctor, last updated June 2024
- Key facts about kidneys. Kidney Care UK. kidneycareuk.org, last updated May 2024
- Dictionary of cancer terms. National Cancer Institute. www.cancer.gov, accessed November 2024
- Chronic kidney disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2024
- Chronic kidney disease. BMJ Best Practice. bestpractice.bmj.com, last reviewed October 2024
- Chronic kidney disease (CKD). Kidney Care UK. kidneycareuk.org, published May 2024
- Chronic kidney disease (CKD). MSD Manuals. msdmanuals.com, last revised October 2023
- Kidney disease stages. Kidney Care UK. kidneycareuk.org, accessed November 2024
- Stage 5 (CKD 5). Kidney Care UK. kidneycareuk.org, accessed November 2024
- Chronic kidney disease (CKD). Medscape. emedicine.medscape.com
- Estimated glomerular filtration rate. National Kidney Foundation. kidney.org, last updated July 2022
- Know your kidney numbers: 2 simple tests. National Kidney Foundation. kidney.org, last updated July 2023
- Renal biopsy. Patient. patient.info/doctor, last updated August 2023
- 10 healthy habits for happy kidneys. Kidney Care UK. kidneycareuk.org, last updated December 2023
- Roxadustat for treating symptomatic anaemia in chronic kidney disease. NICE Guidance. nice.org.uk, published July 2022
- Renal replacement therapy and transplantation. Patient. patient.info/doctor, last updated February 2022
- Michelle Harrison, Freelance Health Editor



