Painful periods (dysmenorrhoea)
- Dr Samantha Wild, Clinical Lead for Women's Health and Bupa GP
Painful periods are common. This pain can be mild for some people. But for others it can be so severe that it affects their day-to-day activities. Some have to take time off work or school.
There are things you can do to help relieve the pain. But if it’s severe and affects your quality of life, you may need to see a GP.
Types of painful period
The medical name for painful periods is dysmenorrhoea (pronounced diss-men-or-ear). You may hear your doctor talk about primary or secondary dysmenorrhoea.
Primary dysmenorrhoea is period pain that isn't caused by a specific condition. It’s more common in teenagers and women under 30. It usually first begins within six to 12 months of your periods starting Pain usually starts at the beginning of your period each month and lasts for between one and three days.Secondary dysmenorrhoea is pain caused by an underlying medical condition. This includes endometriosis or fibroids, for example. This type of period pain usually begins some years after your periods have started, often when you’re in your 30s or 40s. You may have pain at any point in your monthly cycle, but it’s usually worse during a period. It can also worsen as your period goes on and persist for a few days afterwards.
Causes of painful periods
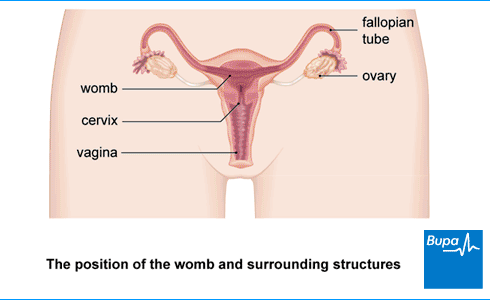
Primary dysmenorrhoea is thought to be caused by prostaglandins, which are hormone-like chemicals. Around the time of your period, the level of prostaglandins in your womb (uterus) increases. This causes the muscles of your womb to tighten. This tightening temporarily reduces the blood supply to your womb, which causes pain.
Causes of secondary dysmenorrhoea include the following.
- Endometriosis is the most common cause of secondary dymenorrhoea. Cells similar to the womb lining grow in other parts of your body such as the ovaries or bowel. They go through the same monthly changes as the womb lining, which can cause pain and inflammation.
- Fibroids are non-cancerous growths in the womb that can cause heavy periods.
- Pelvic inflammatory disease is an infection in your womb that can spread to your fallopian tubes and sometimes your ovaries.
- Adenomyosis is a condition where glands usually found in the womb lining grow into the walls of your womb. Your womb gets slightly larger than it should be, and you may have heavy periods with cramps.
- A copper contraceptive intrauterine device (IUD) can sometimes cause painful periods after the device is fitted.
Pain from an IUD should settle within three to six months. If not, your GP or gynaecologist may suggest that you have the IUD removed and try a different type of contraception. A similar device (called an intrauterine system or IUS) that releases hormones may help with painful periods.
You're more likely to have painful periods if:
- your periods started at a young age
- you have heavy bleeding or long periods
- other women in your family have painful periods
- you've never had children
- you smoke
- you’re very overweight or very underweight
- you are under emotional stress
Symptoms associated with painful periods
Primary dysmenorrhoea usually causes cramping pain in your lower abdomen (tummy). The pain can spread to your lower back and thighs. You may feel this a few hours before and during your period. It usually gets better at the end of your period.
As well as pain, you might have some other symptoms before or during your period. These include:
- tiredness
- feeling or being sick
- diarrhoea
- a headache or feeling light-headed
- bloating
- emotional symptoms
Secondary dysmenorrhoea can also cause abdominal cramping pain. You may also have a feeling of heaviness in your tummy, and back pain. You may have other symptoms, including:
- heavy or irregular periods
- bleeding in-between periods
- an unusual discharge from your vagina
- pain during sex, and you may bleed afterwards
If you have any of these symptoms, contact your GP for advice.
Worried about your Period health?
A personalised care plan for heavy, painful or irregular periods for those 18 and over. Now available.
Diagnosis of painful periods
The GP will ask about your symptoms and about your medical history. They will also ask how your periods affect your day-to-day life. It may help to keep a record of your symptoms that you can show your GP.
If you’re young and haven’t had sex, and your GP thinks you may have primary dysmenorrhoea, they may just examine your tummy. If you’re sexually active or your GP thinks you may have secondary dysmenorrhoea, they’ll probably examine inside your vagina too.
What happens during an internal examination
You can ask to have someone with you during the examination if you want to. First, you remove your lower clothing and lie on your back on the couch with your legs bent and knees apart.
Your GP will put on some gloves and put some lubricant on their fingers. Then they’ll put their fingers into your vagina to gently feel your womb and cervix. At the same time, they’ll use their other hand to press on the lower part of your tummy. This helps them to feel your womb for any abnormal signs. Next, they’ll use a tool called a speculum to gently hold your vagina open while they examine your cervix.
Your GP may also suggest:
- taking a swab from inside your vagina, to check for infection
- blood tests to check for a low level of iron in your blood (anaemia) and other conditions
- an ultrasound scan to look at your womb from the outside, through your tummy
- a transvaginal scan – an ultrasound from the inside, using a device that goes into your vagina. The scan may feel uncomfortable, but it shouldn’t be painful.
If your symptoms are severe or your GP thinks there may be another cause, they may refer you to a gynaecologist. This is a doctor who specialises in women’s reproductive health. Your gynaecologist might recommend that you have other tests such as:
Self-help for painful periods
There’s a lot you can do to help yourself. If your period pain is mild, you can try the following tips but remember it’s always ok to see a doctor if you’re struggling.
- You could use a hot water bottle or heat patch to apply heat to your tummy or back. Don’t put these directly against your skin because you may burn yourself.
- A warm bath or shower may help you relax.
- Gently massaging your tummy or back may help.
- Wearing loose-fitting clothing just before and during your period may help.
- Over-the-counter painkillers such as ibuprofen or paracetamol may help. Your pharmacist will be able to advise on which is best for you.
- A transcutaneous electrical nerve stimulation (TENS) machine may help to ease pain. You place this on your skin, near where you feel the pain. It sends mild electrical signals that help to block pain signals travelling to your brain. You can buy a TENS machine from a pharmacy.
If you smoke, this may increase your risk of period pain. So it may help to ease your symptoms if you stop smoking.
There is some research evidence that regular exercise can help to reduce period pain. The women in these studies exercised for 45 to 60 minutes at least three times a week. You may also find that gentle stretching exercises such as yoga help to ease your symptoms during a period.
Treatment of painful periods
Treatment depends on what’s causing your painful periods and how severe your pain and symptoms are.
If you need it, there are treatments that your GP can prescribe for primary dysmenorrhoea. If you have secondary dysmenorrhoea, they’ll need to find the cause of your symptoms before discussing treatment with you.
Painkillers
Many people use non-steroidal anti-inflammatory drugs (NSAIDs) to treat painful periods. Ibuprofen, which you can buy over the counter, is an NSAID. Your GP might prescribe others such as mefenamic acid.
NSAIDs ease pain and cramping by blocking the production of prostaglandins. For more information about prostaglandins, see our section on causes of painful periods.
Like most medicines, NSAIDs can have side-effects. It’s best to take them with food or a glass of milk. Ask your doctor or pharmacist about any side-effects related to your medicines.
Hormonal contraception
Contraception containing hormones can help to reduce some of your symptoms. Your GP may suggest any of the following:
- the combined contraceptive pill
- progesterone-only pill
- contraceptive injection
- contraceptive implant (for example, Depo-Provera)
- an intrauterine system (IUS; for example, the Mirena coil)
Talk to your GP about the best option for you. Always read the patient information leaflet that comes with your medicine carefully. If you have any questions, ask your pharmacist.
If you are trying to get pregnant, you’ll need a different treatment.
Surgery
If endometriosis is causing your period pain, an excision surgery could remove the unhealthy tissue which may reduce your pain. If you don’t want to have children in the future, you could consider a hysterectomy. This is an operation to remove your womb (uterus). It won’t cure endometriosis, but it can help in some cases. Your gynaecologist will only suggest this as a last resort. First, they’ll see if they can find a specific cause for your painful periods or a treatment that works for you. Talk to your gynaecologist for more information.
Complementary therapies
To ease symptoms of painful periods, some people try complementary therapies alongside treatments their doctors prescribe. Currently, there’s no evidence that herbal medicines or dietary supplements can help.
Researchers have looked at the use of acupuncture. There is some evidence that it may help with period pain, but we need more research to be sure. Some women find therapies that are relaxing – for example, yoga – helpful.
You may have an underlying medical condition, such as endometriosis or fibroids. But sometimes, painful periods aren’t caused by a specific condition. Doctors think the main cause is an increase in chemicals called prostaglandins. These cause the muscles of your womb to tighten. This can temporarily reduce the blood supply to your womb, causing pain.
For more information, see our section on causes of painful periods.
You may be able to ease the symptoms of painful periods with over-the-counter painkillers.
For more suggestions, see our section on self-help for painful periods.
There are also treatments that your GP can prescribe for you.
For more information, see our section on treatment of painful periods.
Primary dysmenorrhoea won’t affect your ability to have children. But secondary dysmenorrhoea might. Pelvic inflammatory disease, fibroids, and endometriosis, can all make it more difficult for some women to get pregnant. If you have any of these conditions, talk to your GP about how this may affect your fertility.
We don’t know for sure, but there is some early research evidence that regular exercise helps to reduce period pains. Do something you enjoy so you’re more likely to keep it up.
For more information, see our section on self-help for painful periods.
Endometriosis
Pelvic inflammatory disease
Pelvic inflammatory disease (PID) is inflammation of the upper part of a woman’s reproductive organs.
Fibroids
Premenstrual syndrome (PMS)
Heavy periods (menorrhagia)
Did our Painful periods (dysmenorrhoea) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Dysmenorrhoea. Patient. patient.info, last updated August 2021
- Period pain. Women's Health Concern. womens-health-concern.org, published November 2022
- Dysmenorrhoea. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2023
- Assessment of dysmenorrhoea. BMJ Best Practice. bestpractice.bmj.com, last reviewed September 2023
- Prostaglandin. Encyclopaedia Britannica. britannica.com, accessed March 2024
- Endometriosis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2023
- Pelvic inflammatory disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised January 2024
- Adenomyosis Clinical Presentation. Medscape. emedicine.medscape.com, updated June 2023
- Contraception – IUC. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised January 2024
- Endometriosis. Patient. patient.info, last updated September 2020
- Dysmenorrhoea Clinical Presentation. Medscape. emedicine.medscape.com, updated November 2021
- Pelvic exam. National Cancer Institute. cancer.gov, accessed February 2024
- Transvaginal ultrasound. Medline Plus. medlineplus.gov, last reviewed April 2022
- Dysmenorrhea Treatment & management. Medscape. emedicine.medscape.com, updated November 2021
- Transcutaneous Electrical Nerve Stimulation. Medscape. emedicine.medscape.com, updated November 2019
- Armour M, Ee CC, Naidoo D, et al. Exercise for dysmenorrhoea. Cochrane Database of Systematic Reviews 2019, Issue 4 Article no. CD004142
- Mefenamic acid. NICE British National Formulary. bnf.nice.org.uk, accessed March 2023
- Non-steroidal anti-inflammatory drugs. NICE British National Formulary. bnf.nice.org.uk, accessed March 2023
- Woo HL, Hae RJ, Pak YK, et al. The efficacy and safety of acupuncture in women with primary dysmenorrhoea. Medicine 2018; 97(23):e11007
- Kanchibhotla D, Subramanian S, Singh D. Management of dysmenorrhea through yoga: A narrative review. Front Pain Res 2023; 4. doi: 10.3389/fpain.2023.1107669
- Liz Woolf, Freelance Health Editor



