Endometriosis
- Dr Madhavi Vellayan, Consultant Gynaecologist
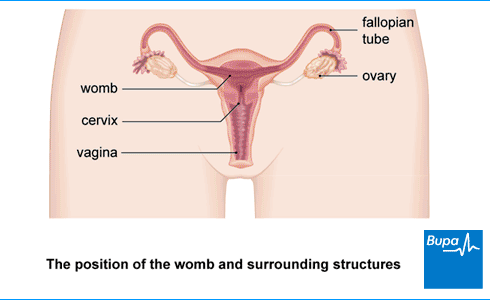
Endometriosis is when cells similar to those in the lining of your womb (uterus) appear in other parts of your body, most commonly in your pelvis. When you have a period, these cells can build up and break away in the same way as your womb lining. This causes painful inflammation in surrounding tissues.
About endometriosis
About one in every 10 people assigned female at birth and of child-bearing age has endometriosis. But it could affect as many as half of people who have infertility. Endometriosis usually stops causing symptoms after the menopause.
Before your period, your womb lining thickens to receive a fertilised egg. If you don’t get pregnant, the lining of your womb breaks down and leaves your body as menstrual blood (a period) each month. This process is controlled by your body’s hormones.
In endometriosis, cells like those that line your womb (endometrial tissue) are also elsewhere in your body. This tissue thickens, breaks down and bleeds with your menstrual cycle. As your body tries to get rid of this endometriosis tissue, the process causes scarring and irritation, and results in pain.
Endometriosis usually affects tissues inside your pelvis. It’s most commonly found in and around your ovaries and fallopian tubes, and the surrounding ligaments. It is also frequently found between your womb and the end part of your bowel (rectum). If you have endometriosis on your fallopian tubes or ovaries, it can lead to fertility problems.
Endometriosis can affect other parts of your body, such as your lungs, but this is rare.
Endometriosis isn’t a type of cancer, and you can’t catch it or give it to anyone else.
Causes of endometriosis
Doctors don’t yet know exactly what causes endometriosis. There are different ideas about how it develops but none of these fully explain why endometriosis happens. It’s probably caused by a combination of things. For example, your immune system or hormones might play a role. Endometriosis may also run in families – you’re more likely to get it if your mother or sister has it.
Some things may increase your risk of getting endometriosis. These include if you:
- started your periods early
- haven’t given birth to any children
- have a low body mass index (BMI)
- have an autoimmune disease (a condition caused by your immune system attacking healthy body tissues)
- smoke
Symptoms of endometriosis
One of the most common endometriosis symptoms is pain in your pelvis, which is usually worse just before and during your period. Endometriosis pain may get worse over time and you may find that it doesn’t get better when you take over-the-counter painkillers such as ibuprofen.
Other endometriosis symptoms include:
- pain during or after sex
- heavy periods
- feeling extremely tired (fatigue)
- difficulty getting pregnant (conceiving)
You may become depressed or anxious because of the long-term pain.
Less common endometriosis symptoms include the following.
- Endometriosis on your bowel can cause pain when you poo (have a bowel movement). You may have blood in your poo during your period.
- If you have endometriosis on your bladder, it can be painful when you pee (pass urine). You may see blood in your pee.
These symptoms can also be caused by conditions other than endometriosis. If you have any of them, see a GP.
Endometriosis symptoms often ease during pregnancy, and they may stop without any treatment.
You might not have any endometriosis symptoms, and only find out that you have endometriosis after tests for something else – for example, infertility.
Diagnosis of endometriosis
Your GP will ask about your symptoms to help make an endometriosis diagnosis. Don’t be embarrassed to tell them about the problems you’re having – including pain during sex or seeing blood when you go to the toilet. It’s important that they know everything.
Your GP may offer you the following tests or refer you to a gynaecologist (a doctor who specialises in women’s reproductive health) for the tests.
Vaginal examination
In a vaginal examination, your doctor will put on some gloves, add some lubricant then insert their fingers into your vagina. They’ll use their other hand to press lightly on your tummy (abdomen) and will gently feel for any abnormalities in and around your womb.
This examination may feel uncomfortable but shouldn’t be painful. Let your doctor know if anything hurts. You can ask to have someone with you while you have this test, if you prefer not to be alone.
Scans
You may have an ultrasound scan, in which a probe will be put into your vagina. This can help to pick up endometriosis or other causes of your symptoms. But there’s a chance that it won’t pick up endometriosis, even if you have it.
You might also be offered a magnetic resonance imaging (MRI) scan. This can help to diagnose endometriosis that’s deep inside your pelvis or that affects your bladder or bowel.
Laparoscopy
It can take time diagnosing endometriosis because the symptoms are similar to other health conditions. The only way doctors can be sure is to check with a procedure called a laparoscopy. You have this under general anaesthetic so you’ll be asleep. Your gynaecologist will look inside your tummy (abdomen) with a laparoscope. This is a narrow tube with an eyepiece that they will put into your tummy through a small cut. They may take a small sample of tissue (biopsy) to send to the lab for examination under a microscope.
If you have a laparoscopy to diagnose endometriosis, your gynaecologist may destroy or remove the endometriosis at the same time. Or they may recommend you have surgery to remove it later. For more information, see our section on treatment.
Sometimes, rather than having this procedure right away, your doctor may suggest you try other treatments first. For example, they might suggest hormonal medicines, to see if they help.
Treatment of endometriosis
Treatment for endometriosis symptoms will depend on how bad your symptoms are, and if you want to have children in the future. Your doctor will discuss the various options with you, and help you decide which endometriosis treatment is best for you.
Pain medicines
Your doctor will probably suggest that you try a non-steroidal anti-inflammatory medicine (NSAID), such as ibuprofen to ease pain and discomfort. Paracetamol is an alternative that you can take alone or with an NSAID. You can buy these pain medicines over the counter from a pharmacy.
If these medicines don’t help, your doctor might prescribe a different medicine for pain.
Always read the patient information leaflet that comes with your medicine. If you have any questions, ask a pharmacist for advice.
Hormone treatments
Hormone treatments can help to reduce areas of endometriosis tissue and so lessen your pain. They aren’t suitable to treat endometriosis if you’re trying to get pregnant because they’re contraceptives. But they won’t have any effect on having children in the future.
Your doctor may offer you the combined oral contraceptive pill. This may be for around six months at first, but if it’s helpful, you can usually continue to take it. If that doesn’t help, or doesn’t suit you, there are two other types of hormonal treatment that your doctor may offer.
- Progestogens. You can take these as tablets, as an injection every three months or in an intrauterine system (coil)
- Gonadotrophin-releasing hormone (GnRH) agonists. You can have these as injections, an implant, or a nasal spray.
Each of these treatments has its own side-effects. Your doctor can explain these and discuss which treatment will suit you best.
Surgery
It’s possible to have areas of endometriosis treated or removed with surgery. If endometriosis affects your fertility, this can help to improve your chance of getting pregnant and can also reduce pain. You have endometriosis surgery under general anaesthesia so you’ll be asleep. Endometriosis can come back after surgery, so you may need to have surgery again in the future.
Laparoscopy (keyhole surgery)
You may have a laparoscopy – a type of keyhole surgery to treat endometriosis. Your gynaecologist will make a small cut and put in a narrow tube with an eyepiece (laparoscope) to look inside your tummy (abdomen). They may be able to see and remove or destroy patches of endometriosis.
Laparotomy (open surgery)
Rarely, if you have severe endometriosis, keyhole surgery may not be suitable. You may need an operation called a laparotomy where a surgeon will make a larger cut in your tummy (abdomen), usually along your bikini line. Your gynaecologist will explain the procedure and why it may be best for you.
Hysterectomy
If you don’t want to have children in the future, your gynaecologist may suggest a hysterectomy. This is a larger operation to remove your womb, and often also your ovaries. This operation can also be done using keyhole surgery.
If you have your ovaries removed, you’re likely to have menopause symptoms afterwards, such as hot flushes. Your specialist may suggest you take hormone replacement therapy (HRT). Talk to your gynaecologist about the pros and cons of this type of endometriosis surgery.
Complications of endometriosis
Complications of endometriosis include the following.
- Scar tissue can attach to organs in your pelvis and tummy (abdomen). These scars are known as adhesions. Adhesions are often already present when you have endometriosis and this can cause pain, but surgery can also increase your risk of getting adhesions.
- You may have difficulty getting pregnant (reduced fertility). This affects around a third of people with endometriosis
- Endometriosis can cause ovarian cysts (called endometriomas or chocolate cysts). These can rupture and cause pain and affect your fertility.
Endometriosis isn’t a cancer and doesn’t cause cancer. Statistically, there’s a slight increase in risk of ovarian cancer, breast cancer and thyroid cancer but the risk is very small.
Speak to a GP or doctor if you have any questions about the complications of endometriosis.
Worried about your Period health?
A personalised care plan for heavy, painful or irregular periods for those 18 and over. Now available.
The symptoms of endometriosis include pain in your pelvis, which is usually worse just before and during your period, and pain during or after sex. Other symptoms include heavy periods and feeling extremely tired. If you’re trying for a baby you might have some difficulty. But some people with endometriosis don’t get any symptoms.
For more information, see our section on symptoms of endometriosis.
If you get your symptoms under control with medicines or surgery, you should be able to live a normal life. Endometriosis can affect everyone differently. In some people, it gets progressively worse whereas in others it stays the same or even improves with time. It can lower your quality of life if the pain affects you at work and in your everyday life, so it’s important to get treatment.
There isn’t a cure so you can’t heal from endometriosis. Endometriosis symptoms often ease during pregnancy, and they may improve without any treatment. And it doesn’t always get worse with time – some studies have shown that endometriosis can reduce in up to a third of people studied.
The best way to treat endometriosis will depend on your individual circumstances. Your doctor will need to consider how bad your symptoms are, and if you want to have children in the future. Treatment options include different types of medicine and surgery. Your doctor will discuss the various options with you, and help you decide which endometriosis treatment is best for you.
For more information, see our section on treatment of endometriosis.
You can’t prevent endometriosis. Studies have looked at whether doing some regular exercise or taking the oral contraceptive pill may prevent endometriosis but didn’t find any proof. Doctors usually recommend a healthy lifestyle, which includes a healthy diet, not drinking too much alcohol and doing some regular physical activity.
Female infertility
Painful periods (dysmenorrhoea)
Gynaecological laparoscopy
In a gynaecological laparoscopy, your surgeon uses a camera (laparoscope) to see inside your lower abdomen (tummy). This means they will be able to see your womb (uterus), fallopian tubes and ovaries.
Hysterectomy
Heavy periods (menorrhagia)
Did our Endometriosis information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
Reviewed by Rachael Mayfield-Blake, Freelance Health Editor, January 2023 Expert reviewer, Dr Madhavi Vellayan, Consultant Gynaecologist Next review due January 2026
- Endometriosis patient information leaflet. Royal College of Obstetricians and Gynaecologists. www.rcog.org.uk, published December 2023
- Endometriosis: diagnosis and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 11 November 2024
- Endometriosis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised November 2024
- Information on endometriosis. European Society of Human Reproduction and Embryology (ESHRE). www.eshre.eu, reviewed 2022
- Endometriosis. Medscape. emedicine.medscape.com, updated 18 July 2023
- Endometriosis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 27 February 2025
- Endometriosis. Patient. patient.info, last updated 18 February 2025
- What is endometriosis? Endometriosis UK. www.endometriosis-uk.org, last reviewed November 2024
- Genital examination in women. Royal College of Nursing. www.rcn.org.uk, last updated 6 November 2023
- Rachael Mayfield-Blake, Freelance Health Editor



