Ovarian cyst removal
- Dr Madhavi Vellayan, Consultant Gynaecologist
Ovarian cysts are fluid-filled sacs that develop in or on your ovaries. For most women, cysts are harmless and go away on their own. But you may need ovarian cyst surgery (cystectomy) to remove a cyst if it’s causing pain or if there’s a chance it could be cancer. .
About ovarian cyst removal
Your doctor will probably suggest you have surgery to remove your cyst if it:
- is large
- is causing symptoms or complications
- doesn’t go away
They‘ll also recommend surgery if there’s a risk your cyst may be ovarian cancer.
There are two ways to carry out surgery to remove an ovarian cyst:
- keyhole surgery (laparoscopy)
- open surgery (laparotomy)
You’re most likely to be offered keyhole surgery, which is usually done as a day-case procedure.
During your operation, your specialist surgeon (gynaecologist) will carry out one on the following procedures:
- remove only the cyst (a cystectomy)
- remove your ovary, fallopian tube, and cyst (a unilateral salpingo-oophorectomy)
- remove both fallopian tubes, both ovaries and the cyst (a bilateral salpingo-oophorectomy)
Your gynaecologist will describe which procedure is best for your personal circumstances.
You can have surgery to remove ovarian cysts when you’re pregnant, but all procedures have some risks and it will depend on your individual circumstances. You may be advised to wait and have the cyst removed after you give birth. Your gynaecologist will explain these risks to you.
Preparation for ovarian cyst removal surgery
Your gynaecologist will explain how to prepare for ovarian cyst removal surgery. For example, if you smoke, they’ll advise you to stop. Smoking increases your risk of getting a chest and wound infection, which can slow your recovery.
Ovarian cysts are usually removed as a day-case procedure. This means you can have the operation and go home on the same day, although you might need to stay overnight.
Before you go into hospital, arrange for friends or family to take you home after your procedure. And ask them to stay at home with you for the first 24 hours.
The operation is done under general anaesthesia, so you’ll be asleep. You’ll need to follow fasting instructions. This means not eating or drinking for a time beforehand – follow your anaesthetist’s advice. You may need to wear compression stockings to help prevent blood clots forming in the veins in your legs. And you may have an injection of a blood thinner medicine.
Your nurse or gynaecologist will discuss with you what will happen before your procedure, including any pain you might have. If you’re unsure about anything, ask. No question is too small. Being fully informed will allow you to give your consent for the procedure to go ahead. Your hospital team will ask you to sign a consent form.
Ovarian cyst removal procedure
Your gynaecologist will talk to you about which type of operation is best for you and if they need to remove more than the cyst.
Keyhole surgery (laparoscopy)
Your gynaecologist will make some small cuts in your tummy (abdomen). One will be near your belly button and there may be two or three lower down, usually on each side. Your doctor will pass small instruments and a tube-like telescopic camera (called a laparoscope) through the cuts. They’ll then examine your ovaries and remove the cyst. They may close the cuts on your skin with glue or stitches.
Open surgery (laparotomy)
Your gynaecologist will make a single, larger cut in your lower tummy (abdomen) to do the operation. Your gynaecologist might have to change from a keyhole surgery to open surgery during the procedure to remove your cyst safely.
Worried about your gynaecological health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0370 218 8122
Aftercare for cyst removal procedure
After keyhole surgery, your nurse will give you painkillers if you need them and let you rest for a few hours. They’ll offer you something to eat and drink. You’ll usually be able to go home later that day when you feel ready.
Before you go home, your nurse will check that you’ve had a pee. They may also give you some painkillers to take home with you. You may be given a date for a follow-up appointment.
You can have a shower or bath the day after the operation. You can take off any dressings then too. Don’t worry about getting the wounds wet, you can gently pat them dry with a towel.
Having a general anaesthetic affects everyone differently. You may find that you’re not so coordinated or that it’s difficult to think clearly. This should pass within 24 hours. In the meantime, don’t drive, drink alcohol, operate machinery or sign anything important. Follow any advice you’re given by your gynaecologist or the hospital.
If your gynaecologist used dissolvable stitches, these will disappear on their own. Other stitches may need to be taken out by the practice nurse at your GP surgery. This will usually be around five to seven days after your operation.
Recovery following ovarian cyst removal
It will take time for your body to recover and heal after an anaesthetic and surgery. Ovarian cyst removal recovery time is different for everyone.
You may feel tired and need to take a daytime nap for a few days after you get home. But it’s important for your recovery to get up and about because this helps to prevent complications from the operation. If you can, try to take a couple of short walks (10 to 15 minutes) in the first few days then build up gradually. By a week after surgery, you may be able to walk slowly and steadily for up to an hour. After about two weeks, you should be back to your normal levels of exercise but take things at your own pace and get advice from your hospital.
You’ll probably be able to go back to work two or three weeks after the operation. If you feel well, and your job isn’t physically demanding, you may be able to start back at work part-time before that. How long it takes for you to recover will also depend on whether you had keyhole or open surgery. Recovery from open surgery takes longer.
If you have any questions about your recovery or when you can get back to your usual day-to-day life, ask your gynaecologist.
If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist.
Side-effects of ovarian cyst removal
Side-effects after ovarian cyst removal should be mostly temporary and may include:
- bruising
- pain or discomfort in your lower tummy for a few days after your operation
- some pain in your shoulders
- a small amount of vaginal bleeding for a few days
- feeling more tired than usual for a few days
Complications of ovarian cyst removal
Most women recover well after ovarian cyst removal. Keyhole surgery causes fewer complications and has a shorter recovery time than open surgery.
Possible complications of ovarian cyst removal include:
- bleeding or a blood clot, usually in a vein in your leg (deep vein thrombosis – DVT)
- an infection
- damage to other organs – for example, your bowel, ureters or bladder – though this uncommon
- a bulge or swelling through your scar; this may be a hernia
Speak to a doctor or contact the hospital where you had your surgery if you have:
- tummy pain that’s getting worse
- a high temperature, especially if you’ve also lost your appetite or you’re being sick
- red or painful skin around your scars
- burning or stinging when you pee, peeing more often or not being able to pee at all
- a painful, swollen, red and hot leg
- chest pain, feeling short of breath or coughing up blood
Alternatives to ovarian cyst removal
If an ovarian cyst isn’t causing any symptoms, your gynaecologist may suggest you don’t have any treatment other than monitoring it. You may need to have regular ultrasound scans to check the cyst and see what size it is. Many cysts disappear on their own without treatment and don’t cause any problems.
Many ovarian cysts disappear without treatment. Depending on the type, it can take between six months and several years for an ovarian cyst to go. If you’re not having treatment, you’ll be asked to have regular ultrasound scans to check the cyst.
For more information, see our section on alternatives to ovarian cyst removal.
If you’ve had a laparoscopy, you’ll probably be able to go back to work two or three weeks after the operation. If you feel well, and your job isn’t physically demanding, you may be able to start back part-time before that. Recovery from open surgery takes longer.
For more information, see our section on recovering from ovarian cyst removal.
Whether or not you’ll need surgery will depend on several things, including the size of the cyst and if it’s growing. You may be offered surgery to remove simple cysts bigger than 10 centimetres across. If you have symptoms or you’re unwell or if there’s a chance it may be cancer, your doctor will also recommend surgery.
For more information, see our section about ovarian cyst removal .
It depends on your individual circumstances. Ovarian cysts are usually removed by keyhole surgery as a day-case procedure and you can go home the same day. In some situations, you may need to have open surgery. This is when a single, larger cut is made and recovery from that will take longer. Sometimes you might need to have more than the cyst removed, for example, your ovary and fallopian tube. This is a bigger operation but could still be done as a keyhole surgery.
For more information, see our section on ovarian cyst removal procedure.
You may get some side-effects after ovarian cyst removal – for example, pain or discomfort in your lower tummy for a few days after your operation. You may have a small amount of vaginal bleeding and feel more tired than usual for a few days too.
For more information, see our section on side-effects of ovarian cyst removal.
Ovarian cysts can be worrying if they’re cancerous (but most aren’t). If you get a complication such as the cyst twisting or rupturing, this is also worrying because it can cause a lot of pain. There isn’t a certain size that makes these complications more likely but, in general, the larger the cyst, the more likely these complications are. Ovarian cysts that get bigger are more likely to need surgery to remove them. But it also depends on if you have symptoms and if there’s a chance the cyst could be cancerous.
Gynaecological laparoscopy
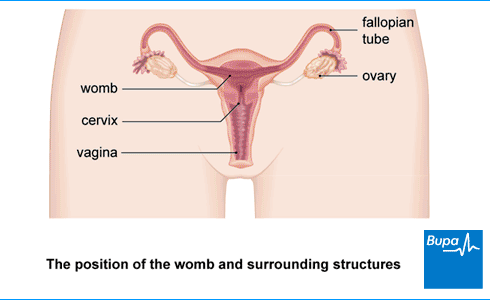
In a gynaecological laparoscopy, your surgeon uses a camera (laparoscope) to see inside your lower abdomen (tummy). This means they will be able to see your womb (uterus), fallopian tubes and ovaries.
Ovarian cysts
Other helpful websites
Discover other helpful health information websites.
Did our Ovarian cyst removal information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Ovarian cysts. BMJ Best Practice. bestpractice.bmj.com, last reviewed 30 October 2023
- Benign ovarian tumours. Patient. patient.info, last updated 27 September 2023
- Mobeen S, Apostol R. Ovarian cyst. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 5 June 2023
- Ovarian cysts. Target Ovarian Cancer. targetovariancancer.org.uk, last reviewed August 2022
- You and your anaesthetic. Royal College of Anaesthetists. www.rcoa.ac.uk, published April 2023
- Laparoscopy – recovering well. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, published 22 October 2015
- Caring for someone recovering from a general anaesthetic or sedation. Royal College of Anaesthetists. www.rcoa.ac.uk, reviewed November 2021
- Ovarian cystectomy. Medscape. emedicine.medscape.com, updated 9 March 2023
- On the day of your operation. Royal College of Anaesthetists. www.rcoa.ac.uk, published 1 March 2021
- Operative laparoscopy. Medscape. emedicine.medscape.com, last updated 25 September 2023
- Scott MJ, Aggarwal G, Aitken RJ, et al. Consensus guidelines for perioperative care for emergency laparotomy Enhanced Recovery After Surgery (ERAS) society recommendations part 2-emergency laparotomy: intra- and postoperative care. World J Surg 2023; 47(8):1850–80. doi: 10.1007/s00268-023-07020-6
- Anaesthesia explained. Royal College of Anaesthetists. www.rcoa.ac.uk, published 1 March 2021
- Common postoperative complications. Patient. patient.info, last updated 28 November 2023
- Diagnostic laparoscopy. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, published June 2017
- Ovarian cysts. Medscape. emedicine.medscape.com, updated 9 March 2023
- Urinary tract infection in adults. Patient. patient.info, last updated 31 March 2023
- Rachael Mayfield-Blake, Freelance Health Editor



