Ovarian cysts
- Dr Madhavi Vellayan, Consultant Gynaecologist
Ovarian cysts are fluid-filled sacs that develop in or on your ovaries. They’re quite common and you can get ovarian cysts at any age. Most ovarian cysts don’t cause any symptoms. They’re usually non-cancerous (benign), and may go away without treatment. But sometimes you may need surgery to remove an ovarian cyst.
Types of ovarian cyst
There are different types of ovarian cyst. These can be split into two groups: functional cysts and pathological cysts.
Functional cysts
Most ovarian cysts are functional cysts. This means that they develop as part of your usual menstrual cycle. New cysts don’t usually develop after the menopause. If you are found to have cysts after the menopause, they probably formed in the stage just before you entered the menopause (perimenopause).
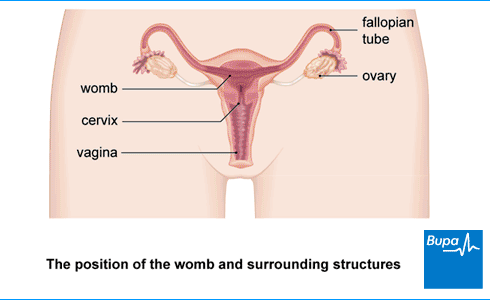
Each month, your ovary produces several follicles (tiny fluid-filled sacs). One of these will mature and release an egg. After releasing the egg, the follicle normally changes into something called the corpus luteum. This releases hormones that help the lining of your uterus (womb) prepare for pregnancy. If the egg isn’t fertilised, the corpus luteum begins to break down.
The two main types of functional cyst form at different stages in this cycle.
- A follicular cyst can happen if a follicle doesn’t release an egg but carries on growing.
- A corpus luteum cyst can form if the corpus luteum doesn’t break down. It may continue to grow and become filled with blood (haemorrhagic cyst).
Pathological cysts
These may happen because of an overgrowth of cells. You may hear these types of ovarian cyst referred to as tumours. But this doesn’t necessarily mean that they’re cancerous. Most aren’t.
You can also get pathological cysts on your ovaries if you have endometriosis or polycystic ovary syndrome (PCOS).
Causes of ovarian cysts
Most ovarian cysts form in response to hormonal changes in your body. So, things that affect your hormone levels can sometimes lead to cysts forming. Such things include:
- using progestogen contraception – this includes the progestogen-only pill, the intrauterine system (the coil – for example, Mirena) and the contraceptive implant
- being pregnant
- taking hormones used to treat infertility
- taking hormone therapy (tamoxifen) – for instance, for breast cancer
- having an underactive thyroid
You can also get ovarian cysts if you have endometriosis.
Other things that can increase your risk of developing ovarian cysts include:
- smoking
- obesity
Symptoms of ovarian cysts
Most ovarian cysts don’t cause any symptoms, so you may not realise you have one. But, depending on the type you have, ovarian cyst symptoms may include:
- pain or discomfort in your tummy (lower abdomen)
- this may be constant or come and go
- it may be a sharp pain or a dull ache
- it may be a dragging aching feeling in your pelvis
- pain during sex
- feeling or looking bloated
- needing to pee more often or urgently
- finding it more difficult to poo
- feeling pressure in your bottom that makes you feel you need to go to the toilet
- getting indigestion or heartburn or feeling very full after you eat
- having painful periods or a change in the pattern of your periods
These can be symptoms of other problems as well as ovarian cysts. If you have any of these symptoms or are worried, contact your GP for advice. For information about ovarian cyst symptoms that need urgent medical help, see our section on complications.
Diagnosis of ovarian cysts
Most ovarian cysts don't cause any symptoms, so you may only find out you have one if you have certain tests – for example, an ultrasound scan.
If you do have symptoms and go to see your GP, they’ll ask you to describe your symptoms. They may also ask if you have any other symptoms. They’ll examine your tummy (abdomen) and may do a vaginal examination at the same time.
Your GP may recommend the following tests.
- Transvaginal ultrasound. An ultrasound probe will be gently inserted into your vagina to produce a clear picture of your ovaries.
- Transabdominal ultrasound. This is a scan over your lower tummy to check for any problems around your pelvic area.
- Blood tests to help rule out cancer, including a test for a substance called CA-125. Your level of CA-125 can be high if you have ovarian cancer, but it may also be raised for other reasons.
Depending on the results, your GP may refer you to a gynaecologist – a doctor who specialises in women’s reproductive health.
Treatment of ovarian cysts
If you have an ovarian cyst, you may not need any treatment. Whether or not you need ovarian cyst treatment will depend on:
- the type of cyst
- how large it is
- if you have symptoms
- your age
- your blood test results
- if there’s a chance the cyst could be cancerous
Your personal preferences will also be considered.
'Watchful waiting'
If your ovarian cyst is small and isn’t causing any problems, your doctor may suggest keeping a close eye on it for a while with ultrasound scans. This is called ‘watchful waiting’. You’ll have another ultrasound scan after a few months to see if there is any change in the cyst. Most small cysts on your ovaries disappear on their own and don't cause any problems. So, this approach helps you avoid having treatment you don’t need.
Your doctor will discuss with you when you should have a repeat ultrasound scan. This may be:
- after a year if you’re still having periods
- every four to six months for a year if you’ve been through the menopause
The timing of the ultrasound scan will depend on your blood test results, type of cyst, your age and symptoms.
You may also have another blood test for CA-125. If your ovarian cyst doesn’t go away, your gynaecologist may then recommend surgery to remove it. This will depend on the type of cyst you have, how much it’s grown, your symptoms and blood test results.
Pregnancy
Ovarian cysts during pregnancy nearly always go away without treatment. Your specialist doctor (obstetrician) will usually only recommend surgery if the cyst is causing symptoms or there’s a risk of cancer.
You’ll normally be offered another ultrasound scan around six weeks after you have given birth, to check if the cyst has disappeared on its own.
Surgery
If your cyst is large, causes symptoms or complications or doesn’t go away, your doctor will probably suggest you have surgery to remove it. They‘ll also recommend surgery if there’s a risk your cyst may be ovarian cancer.
There are two ways of carrying out surgery for an ovarian cyst:
- Keyhole surgery (laparoscopy). This means a surgeon performs the procedure through small cuts (incisions) in your tummy. It can be a safer alternative to open surgery, which involves making a larger cut to open your tummy. It’s usually associated with fewer complications and a shorter recovery time.
- Open surgery (laparotomy). This means making a bigger cut in your tummy.
You’re most likely to be offered keyhole surgery, which is usually done as a day-case procedure.
Complications of ovarian cysts
Having an ovarian cyst doesn’t usually cause any serious problems. But there are two main complications of ovarian cysts.
- Ovarian torsion. This is when the cyst causes your ovary to twist, which cuts off the blood supply to your ovary. You’ll likely get sudden severe tummy pain. Ovarian cyst torsion is more common with larger cysts (over 4 cm) and if you haven’t been through the menopause yet.
- Ruptured ovarian cyst. This is when the cyst suddenly bursts or haemorrhages, often for no reason, but sometimes during exercise or other physical activity. Ruptured ovarian cyst symptoms include sudden, severe tummy pain and feeling sick. You may also be sick, and you may faint.
If you have been diagnosed with an ovarian cyst and get sudden, severe lower tummy pain, go to your nearest A&E department straightaway. You may need to have surgery.
Although most ovarian cysts are benign, there’s a potential risk they may be or may become cancerous. Your doctor will monitor and check for cancer.
Living with endometriosis? Looking for support?
The endometriosis support page in our Women's Health Hub offers a wide range of expert advice, information and tools.
Although rare, ovarian cysts can cause complications that can be serious if not treated promptly. These include ovarian rupture and torsion, which are considered medical emergencies. You’ll likely get sudden severe tummy pain with both of these complications. And you may also feel sick if you have a ruptured ovarian cyst. Go to accident and emergency if you get these symptoms.
For more information, see our section on complications of ovarian cysts.
Most ovarian cysts don’t cause any symptoms and go away without treatment. Whether or not you need ovarian cyst treatment will depend on things like the type of cyst you have and how large it is. You may also need treatment if you have symptoms and have been through the menopause.
For more information, see our section on treatment of ovarian cysts.
Most ovarian cysts don’t cause any symptoms but if you do get symptoms, they may include pain or discomfort in your tummy (lower abdomen). This may be a constant pain or it may come and go. And it may be a sharp pain or a dull ache. Sex may also be painful. And you may feel or look bloated or have a dragging aching feeling in your pelvis.
For more information, see our section on symptoms of ovarian cysts.
Most ovarian cysts develop naturally as part of your menstrual cycle. Others may develop because of an overgrowth of cells. They usually form because of hormonal changes in your body. Ovarian cysts can also be caused if you have another health condition such as endometriosis.
For more information, see our sections on types and causes of ovarian cysts.
Polycystic ovary syndrome (PCOS)is the name given to a collection of symptoms caused by abnormalities in the way your body produces and manages sex hormones. The small cysts you get on your ovaries if you have PCOS are actually fluid-filled bags that contain an egg (follicles). They’re follicles on your ovaries, not cysts.
Many women have one or more cysts on their ovaries at some point in their lives but these can have various causes. They often don’t cause any symptoms and go away without treatment.
For more information, see our section on causes of ovarian cysts.
Ovarian cysts don’t usually cause weight gain. But feeling bloated can be a symptom of having an ovarian cyst. This might make you feel as though you’ve put on weight.
If you have polycystic ovary syndrome (PCOS), you may put on weight as part of that condition.
For more information, see our section on symptoms of ovarian cysts.
Ovarian cyst removal
Polycystic ovary syndrome (PCOS)
Ultrasound
Ultrasound is a type of scan that uses sound waves to produce images of the inside of your body
Did our Ovarian cysts information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Ovarian cysts. BMJ Best Practice. bestpractice.bmj.com, last reviewed 30 October 2023
- Mobeen S, Apostol R. Ovarian cyst. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 5 June 2023
- Benign ovarian tumours. Patient. patient.info, last updated 27 September 2023
- Ovarian cysts. Medscape. emedicine.medscape.com, last updated 9 March 2023
- Female reproductive endocrinology. MSD Manuals. msdmanuals.com, reviewed/revised April 2022
- Desogestrel. NICE British National Formulary. bnf.nice.org.uk, last updated 1 November 2023
- Levonorgestrel. NICE British National Formulary. bnf.nice.org.uk, last updated 1 November 2023
- Etonogestrel. NICE British National Formulary. bnf.nice.org.uk, last updated 1 November 2023
- The management of ovarian cysts in postmenopausal women. Royal College of Obstetricians and Gynaecologists. www.rcog.org.uk, last updated 3 August 2022
- Ovarian cyst rupture. Medscape. emedicine.medscape.com, updated 9 March 2023
- Polycystic ovarian syndrome. Medscape. emedicine.medscape.com, updated 27 November 2023
- Polycystic ovary syndrome. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2023
- Laparoscopy. Encyclopaedia Britannica. www.britannica.com, accessed 28 February 2024
- Rachael Mayfield-Blake, Freelance Health Editor



