Heavy periods (menorrhagia)
- Dr Madhavi Vellayan, Consultant Gynaecologist
Heavy periods (menorrhagia) mean that your blood loss during your period is so heavy that it interferes with your daily life. Heavy periods are common and are more likely to develop as you get older.
About heavy periods (menorrhagia)
The amount of blood you lose during a period varies from person to person but you’ll usually lose between 25ml and 80ml of blood. When your periods are heavy, you lose more than 80ml of blood each period or you bleed for more than seven days.
You may have heavy periods all the time or just during certain times in your life – for example, at puberty or just before the menopause. They’re most common in women aged between 30 and 49.
Your doctor will ask you what impact your heavy periods have on your life. If they affect your quality of life, you may need treatment.
Causes of heavy periods (menorrhagia)
Your heavy periods may not have a specific cause. This means there’s no obvious disease or physiological issue that causes them. Heavy periods without a cause are known as primary menorrhagia. Sometimes, heavy periods are the result of a condition or disease. Heavy periods caused by a disease are called secondary menorrhagia. Conditions that can cause heavy periods include:
- fibroids or polyps (growths of tissue) in your womb
- polycystic ovary syndrome (PCOS)
- adenomyosis – when cells that normally line your womb grow into the muscle wall as well
- endometriosis – when cells that normally line your womb grow in other parts of your body
- an infection such as pelvic inflammatory disease (PID)
- other health conditions – for example, an underactive thyroid, liver disease, kidney disease
- cancer – for example, in your ovaries or womb
You can also get heavy periods if you use a copper-containing intrauterine contraceptive device (IUD or coil).
Symptoms of heavy periods (menorrhagia)
The main symptom of heavy periods is losing more than 80ml of blood at each period. It’s obviously difficult to measure this. Signs that you’re losing too much blood during your period include:
- you need to use change sanitary pads or tampons at least every three hours on your heaviest days or need to change your menstrual cup more than recommended
- you use two methods of sanitary products together – for example, a tampon and a towel at the same time or you use two towels to prevent leaks
- you pass blood clots, which can sometimes be painful
- you bleed through to your clothes or bedding – this is called flooding
Heavy bleeding can affect your usual activities and interfere with your work and social life, your relationships and leisure time.
You may also have symptoms such as pain or discomfort alongside heavy bleeding.
Signs that your heavy periods are caused by an underlying condition include:
- bleeding between periods or after you have sex
- pain after you’ve had sex or before your period or pain that doesn’t go away
- a feeling of pressure in the lower part of your tummy (abdomen)
If you have any of these symptoms, contact your GP.
Diagnosis of heavy periods (menorrhagia)
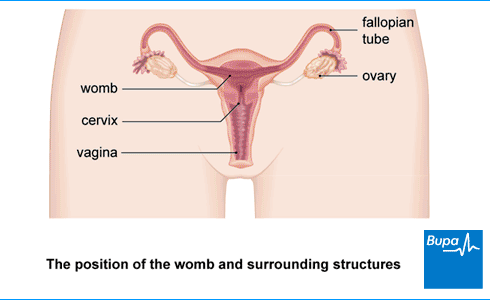
Your GP will ask about your symptoms and medical history, and how the heavy bleeding affects you. They may examine your tummy. And your GP may do an internal examination. This is to look at the neck of your womb (cervix). Your GP may also do a ‘bimanual examination’. In this test, they’ll put their fingers into your vagina (they’ll wear gloves) and press on your tummy at the same time with their other hand. This is to check for tenderness and changes to your womb (uterus).
You might need to have some other tests, which may include the following.
- A blood test to check for anaemia and to see how well your blood clots.
- A pregnancy test to check if your bleeding is a complication of being pregnant.
- An ultrasound scan, which produces images of the inside of your tummy and your womb.
- A hysteroscopy, which is a procedure to look inside your womb. Your doctor may also take a sample of your womb lining. This is called an endometrial biopsy.
Treatment of heavy periods (menorrhagia)
The main aim of treatment for heavy periods is to improve your symptoms and quality of life. There are several treatments for heavy periods. Talk to your doctor about the pros and cons of each, so you can decide what might be the best option for you. The treatment you have will depend on whether or not you have any health conditions such as fibroids, and if you plan to have children. Your GP can prescribe some treatments, but they may also refer you to see a specialist.
If there’s a particular condition that’s causing your heavy bleeding, treatment for that may ease your symptoms.
Levonorgestrel intrauterine devices (LNG-IUDs)
An LNG-IUD is a small, plastic device that’s put into your womb and slowly releases a hormone called levonorgestrel (a progesterone hormone). Hormones are chemical messengers in the body. Levonorgestrel reduces the lining of your womb, which makes it thinner, so you should bleed less.
The LNG-IUD works as a contraceptive as well as a treatment for heavy periods. You usually keep it in for three to six years, depending on the type of device you have.
If the perimenopause (time just before the menopause) is causing your heavy periods, the LNG-IUD may be useful for you. This is because it offers you a form of progesterone that can reduce bleeding.
The LNG-IUD is different from an intrauterine contraceptive device (IUD or coil), which can make heavy periods more likely.
Medicines
Medicines can reduce the amount of bleeding you have and ease your symptoms. The main medicines used to treat heavy periods are:
- tranexamic acid
- non-steroidal anti-inflammatory drugs (NSAIDs) such as mefenamic acid
- the combined or progesterone-only contraceptive pill
If you have anaemia from heavy bleeding, you might need to take iron tablets.
Always read the patient information leaflet that comes with your medicine. If you have any questions, ask a pharmacist or GP for advice.
Uterine artery embolisation
This is a possible treatment choice if your heavy periods are caused by fibroids. Your doctor will put a thin tube into an artery in your wrist or groin and move it until it reaches the blood vessels that supply the fibroids. They’ll inject a chemical that blocks these blood vessels and so shrinks the fibroids.
Surgery
You may need to have surgery if other treatments haven’t worked. There are three main types of surgery that can treat heavy periods.
- Endometrial ablation is an operation to destroy or remove most of your womb lining. If you want to have children in the future, this treatment is unlikely to be a good option for you.
- Myomectomy is an operation to remove fibroids without removing your womb. Your doctor may suggest this if you want to have children in the future.
- Hysterectomy is an operation to remove your womb and it’s the only complete cure for heavy periods. It’s a major operation, so is usually only an option if all other treatments haven’t worked. After a hysterectomy, you won’t have periods and you won’t be able to have children.
Complications of heavy periods (menorrhagia)
Heavy periods can cause iron-deficiency anaemia. This is when you have too few red blood cells, which means your blood carries less oxygen than you need. This can make you feel tired, out of breath and give you a headache. Heavy periods are the most common cause of iron-deficiency anaemia.
Heavy periods can be distressing and have a major impact on your daily life. You may find that you’re less likely to play sport, exercise or go out when you have your period. The impact of such heavy periods can affect your mood and mental health, so it’s important to get help from your GP.
Worried about your Period health?
A personalised care plan for heavy, painful or irregular periods for those 18 and over. Now available.
Most women with heavy periods will be able to get pregnant. But some of the causes of heavy bleeding can make it more difficult. These include causes such as fibroids and pelvic inflammatory disease. Tell your doctor if you're trying to get pregnant or want to have children in the future because it will affect your treatment choices.
In a normal period, you can expect to lose between 25 and 80ml of blood. But if your periods are heavy, you lose more than 80ml of blood each period or you bleed for more than seven days. It’s obviously difficult to know but there are signs that you’re losing too much blood during your period. For example, you may need to change sanitary pads or tampons frequently or use two methods of sanitary protection together to prevent leaks.
For more information, see our section on symptoms of heavy periods.
You won’t usually need to go to A&E with heavy periods. But if you feel weak, dizzy or short of breath, and have heavy menstrual bleeding, seek urgent medical attention. The hospital team will try to reduce or stop the bleeding with medicines such as progestogen or tranexamic acid. It’s possible you may need a hysterectomy. Your doctor will explain what is the best treatment is for you.
Periods can get heavier as you age. Heavy bleeding is most common in women aged between 30 and 49 years. Heavy periods without any known cause can be more common just before the menopause. Menopause can happen any time but usually when you’re between 45 and 55.
You can take treatments to try and stop a heavy period. You can try an LNG-IUD, which is a small, plastic device that’s put into your womb. It slowly releases a hormone that should make you bleed less. Medicines like tranexamic acid can reduce the amount of bleeding you have and ease your symptoms. Contraceptive pills and injections can also stop periods. Surgery such as a hysterectomy can cure heavy periods if other treatments have failed.
For more information, see our section on treatment of heavy periods.
Related information
Endometrial ablation
Endometriosis
Fibroids
Did our Heavy periods (menorrhagia) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Heavy menstrual bleeding: assessment and management. National Institute for Health and Care Excellence (NICE). nice.org.uk, last updated 24 May 2021
- Menorrhagia. Patient. patient.info, last updated 20 May 2020
- Menorrhagia (heavy menstrual bleeding). NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised March 2023
- Walker MH, Coffey W, Borger J. Menorrhagia. StatPearls publishing. www.ncbi.nlm.nih.gov, last updated 11 March 2023
- Fibroids. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2022
- Assessment of abnormal uterine bleeding. BMJ Best Practice. bestpractice.bmj.com, last reviewed 20 August 2023
- Endometriosis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 20 August 2023
- Pelvic inflammatory disease. BMJ Best Practice. bestpractice.bmj.com, last reviewed 20 August 2023
- Gynaecology. Oxford Handbook of General Practice. Oxford Medicine Academic. academic.oup.com, published online June 2020
- Pelvic examination technique. Medscape. emedicine.medscape.com, updated 21 October 2022
- Contraception – IUC. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2023
- Anaemia – iron deficiency. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2023
- Uterine artery embolisation/uterine fibroid embolisation. British Fibroid Trust. britishfibroidtrust.org.uk, last updated 1 February 2021
- Bofill Rodriguez M, Lethaby A, Fergusson RJ. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database of Systematic Reviews 2021, Issue 2. doi: 10.1002/14651858.CD000329.pub4
- Pelvic inflammatory disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2023
- Melendez Rivera JG, Anjum F. Hypovolemia. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 27 April 2023
- Rachael Mayfield-Blake, Freelance Health Editor



