Gastric bypass surgery
Your health expert: Mr Peter Lamb, Consultant General and Upper Gastrointestinal Surgeon
Content editor review by Liz Woolf, Freelance Health Editor, June 2023.
Next review due June 2026.
You may have gastric bypass surgery to help you lose weight if you’re very overweight. The surgery makes your stomach smaller and bypasses part of your bowels (intestines). Losing weight can help to improve any weight-related health problems you have.
About gastric bypass surgery
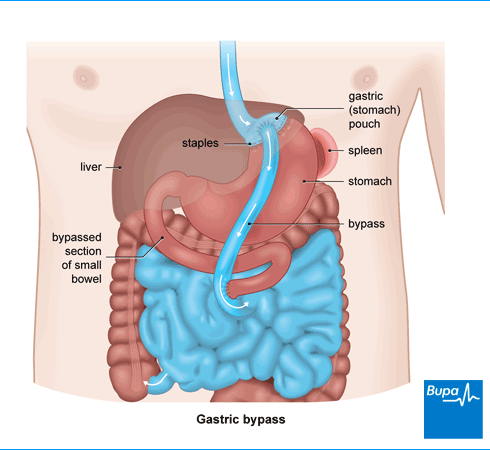
In gastric bypass surgery, you have part of your stomach sectioned off and connected directly to your small bowel. Then, food you eat will bypass most of your stomach and the first part of your small bowel. You’ll feel fuller after eating smaller amounts of food. The surgery also changes hormone signals that pass between your bowel and your brain, controlling your appetite.
You may hear this operation called a ‘Roux-en-Y’. This is just the name of the method surgeons most often use to carry it out.
Gastric bypass surgery can help you lose up to two-thirds of your excess weight. You are likely to lose most weight in the first year after surgery and the rest in the following six months to a year. You should be able to keep most of this weight off permanently. But this depends on sticking to some major changes to your lifestyle after the operation. For example, you’ll need to:
- change your diet – stop snacking and choose healthier options
- not drink too much alcohol
- take regular exercise
Your doctor will talk through these changes with you.
Who can have gastric bypass surgery?
Your GP may refer you to a specialist team to discuss your options. This is the weight-management service and includes a surgeon, dietitian, and psychologist. They will assess you to see if gastric bypass surgery is right for you. They may suggest weight loss surgery if you:
- have a body mass index (BMI) of 40 or more
- have a BMI over 35, with or without a condition that could improve if you lose weight (for example, type 2 diabetes or high blood pressure)
- are fit enough to have an anaesthetic and surgery
- are committed to having long-term follow-up appointments
- commit to changing your lifestyle and diet after your operation
- are over 18 (although children may have this surgery in exceptional circumstances)
You can usually only have this surgery if you’ve tried to lose weight in other ways and this hasn’t worked. If you don’t meet the criteria for NHS funding, you may be able to have the surgery privately.
Preparation for gastric bypass surgery
Your hospital will let you know how to prepare for your operation.
If you smoke, you’ll be asked to stop at least six weeks before the operation. Smoking increases your risk of complications after surgery.
Your surgeon may ask you to eat a low-fat, low-carbohydrate diet for two weeks before surgery. This is to shrink your liver, which allows your surgeon better access to your stomach.
You have gastric bypass surgery under a general anaesthesia (GA), so you’ll be asleep during the operation. You won’t be able to eat or drink for some time before surgery. Your doctors will tell you what to do and it’s important to follow their advice.
You surgeon will ask you to wear compression stockings after the operation. This helps to prevent blood clots forming in the veins in your legs (deep vein thrombosis). You may also have injections of an anti-clotting medicine.
Your surgeon will discuss with you what will happen before, during and after your surgery. If you’re unsure about anything, don’t be afraid to ask. No question is too small. It’s important that you feel fully informed, so you feel happy to give your consent for the operation to go ahead. You do this by signing a consent form.
Gastric bypass surgery
A gastric bypass operation usually takes around one to two hours. But this can vary between hospitals.
Most surgeons use keyhole (laparoscopic) surgery. This means your surgeon makes several small cuts in your tummy rather than one large cut. They put small instruments through the cuts and guide them using a telescope with a camera. Sometimes your surgeon may start with keyhole surgery, but find they need to switch to open surgery.
During the operation, your surgeon staples across the top of your stomach, to form a small pouch. They then make an opening in the pouch and connect it directly to your small bowel. Food passing through will then bypass the lower part of your stomach and the first part of your small bowel. The surgeon reconnects the first part of your small bowel further down. This means the juices from your stomach, pancreas and liver can mix with the food so that you can absorb enough nutrients after your surgery.
Your surgeon will close your cuts with stitches or small metal clips and cover them with a dressing.
Bupa Weight Management Plan
The Bupa weight management plan is designed for people with a BMI over 30 (or over 27 if you have a weight related condition). The plan is designed to empower you to achieve and maintain a healthy weight in a sustainable way.
To book or to make an enquiry, call us on 03452660566∧
Aftercare for gastric bypass surgery
After surgery, you’ll need to rest until the anaesthetic has worn off. But it’s important to get out of bed and move around as soon as you can. This helps you to recover and prevents blood clots developing in your legs. Your doctor will have made sure you have painkillers prescribed.
Your hospital will take measures to help prevent deep vein thrombosis (DVT). You may have to wear compression stockings. Or you may have an intermittent compression machine that inflates and deflates around your legs. Both of these aim to boost the blood circulation in your legs. You may also continue to have anti-clotting injections, such as heparin.
At first, you’ll have a drip inserted into a vein in your hand or arm to give you fluids. When you feel well enough, you can start to drink small amounts of water. Your nurse will then remove the drip.
Going home
You’ll usually be able to go home a day or two after your operation. Ask a friend or family member to drive you. Before you go home, your nurse will tell you how to care for your wounds and give you a follow-up appointment. You may need to take painkillers for a few days after the operation.
Everyone recovers at their own rate, but it’s sensible to allow up to six weeks to recover fully from a gastric bypass operation. You usually go home on a liquid diet – your surgeon will give you advice on how to move on from this. There’s more information on diet below, in our section on lifestyle changes.
Lifestyle changes after surgery
You have to make major changes to your diet after gastric bypass surgery, as your stomach will be smaller. You have a liquid diet for the first couple of weeks after going home. Then you move on to puréed, then mashed food. By six weeks after your operation, you should be having several small solid meals a day.
It can be difficult to drink enough. You need at least one and a half litres a day to stay healthy. Drink slowly and between meals or it will fill you up too much.
You need to make sure that you get enough protein every day. If you don’t, it can affect your health. Your doctor is likely to suggest a low-fat, high protein diet.
It’s difficult to get enough vitamins and minerals from your diet after gastric bypass. So you’ll need to take a complete multivitamin supplement for the rest of your life. You may also have regular vitamin B12 injections. Your doctor will arrange regular blood tests to check you’re getting everything you need.
You’ll need to do more exercise and drink less alcohol too. This will help you to get the most from your gastric bypass operation, so you can lose excess weight and keep it off.
Losing weight after a gastric bypass is usually a positive thing. But you may find it hard to adapt to your lifestyle and appearance after the operation. Talk to your GP or surgeon if you’re struggling to cope. They may suggest a patient support group. There you can get advice from other people who have been through the same operation.
Side-effects of gastric bypass surgery
You may have some bruising around your wounds after a gastric bypass. But this shouldn’t last more than a week or two.
You may feel sick or even be sick after eating. This is because you’ll only be able to eat a small amount of food at a time. This should get better with time as you get used to eating smaller amounts.
You may get an unpleasant side-effect called dumping syndrome if you eat too many sugary foods. It can make you feel sweaty, sick and lightheaded. You may also feel very tired and have tummy pain and diarrhoea. Symptoms can come on 30 minutes to an hour after you eat (early dumping), or within three hours (late dumping). It may help to:
- eat smaller more frequent meals that are low in carbohydrates, especially sugar
- don’t drink during meals or for half an hour afterwards
- cut down or cut out dairy products
- rest for half an hour after eating
Ask your dietitian or doctor for more advice.
Complications of gastric bypass surgery
There can be complications with any surgery, such as a wound or chest infection or a blood clot. To reduce the risk of these, it’s best to follow the advice of your nurse, doctor, and physiotherapist. This will include getting up and moving as soon as possible after surgery and doing breathing and leg exercises.
Gastric bypass complications can happen soon after surgery or some months later. Early complications happen within a month of surgery. They include bleeding or a leak from the stomach or bowel. This is most likely where the stomach has been stapled or your small bowel rejoined. If you have abdominal or shoulder pain, see signs of blood when you’re sick, or your poo looks black like tar, contact your surgeon or hospital.
Later complications can include the following.
- Gallstones – this can happen in up to one in three people having this type of operation.
- An internal hernia – part of the small bowel can get twisted at the site of the operation, causing pain.
- Stomach ulcer – you may have medicine to reduce stomach acid to help prevent this. Ulcers are more common in smokers.
- A stricture – this is narrowing of the join between your stomach pouch and small bowel. you may feel sick, or be sick.
If you have pain, sickness that doesn’t go away, or any other concerns after your surgery, contact your surgeon for advice.
These complications may sound frightening, but, apart from gallstones, they are uncommon, particularly after keyhole surgery. Ask your surgeon to talk them through with you. They will be able to give you more information about how likely they are in your case.
What you need to know before gastric bypass surgery
Gastric bypass surgery is a major operation with potentially serious complications. But it does also have many benefits. It’s important to discuss the surgery thoroughly with your doctor or surgeon beforehand. Then you can make an informed decision about whether to go ahead.
Benefits
Your doctor may suggest gastric bypass surgery to improve your overall health. Afterwards, you are less likely to have:
- diabetes – your doctor may suggest surgery as it can reverse type 2 diabetes in many people
- breathing disorders such as sleep apnoea
- a heart attack or stroke
- back pain and joint problems such as osteoarthritis
- high blood pressure
- weight-related cancers, such as womb cancer
For some people, the surgery can help their mental health, with improved quality of life and less depression.
Drawbacks
You might not lose enough weight after gastric bypass surgery, or put weight back on later. Some people find it difficult to adapt to diet advice and lifestyle changes. Your surgeon will discuss this with you and help support you.
You’ll need at least two years of medical care and check-ups after your surgery. The changes to your lifestyle, along with what and how much you eat, are life-long commitments. You will also need to take vitamin and mineral supplements for the rest of your life.
Some people are disappointed with how they look after their operation. This is often because they’re left with excess skin. Some people need further surgery to remove this. It’s important to have realistic expectations, so talk to your surgeon beforehand.
Alternatives to gastric bypass surgery
Other types of surgery can help you lose excess weight. These include sleeve gastrectomy and gastric band surgery. As with gastric bypass surgery, you need to make long-term changes to your diet and lifestyle.
Another option is to have a silicon balloon inflated in your stomach. This will make you feel full but it can only be used short term.
Ask your surgeon about the options available – they’ll help you decide which one is best for you.
You’ll start losing weight as soon as you’ve had gastric bypass surgery. Most people lose most of their excess weight in the first year. Weight loss can carry on after that, but will usually tail off in the second year as your weight settles.
See our section about gastric bypass surgery for more information.
Dumping syndrome is a possible side-effect of weight loss surgery. It can happen if you eat too much sugar. The stomach empties too quickly, which can cause sickness, dizziness and light-headedness.
There is more information in the section on gastric bypass surgery side-effects .
The weight you lose in gastric bypass surgery can make your skin loose, leaving you with folds of excess skin. Cosmetic surgery can remove this but it’s best to wait until your weight is stable. This could be up to two years after your bypass surgery.
Gastric band operation
Gastric band surgery is a common type of weight loss (bariatric) surgery for people who are very overweight (obese).
Tips for a healthy and well-balanced diet
A healthy, well-balanced diet involves eating foods from a variety of food groups to get the nutrients that your body needs to function.
Tools and calculators
BMI calculator
BMI, or body mass index, is one way of measuring whether you’re a healthy weight for your height.
Simply enter your details into our calculator and the result will give you an indication of whether you're a healthy weight.
Calories calculator
If you want to lose weight, you need to increase your physical activity and watch your calorie intake. Bupa's calorie calculator will help you to work out how many calories you're burning in a day.
Other helpful websites
Discover other helpful health information websites.
Did our Gastric bypass surgery information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Obesity in adults. BMJ Best Practice. bestpractice.bmj.com, last updated June 2023
- Oxford Handbook of Endocrinology and Diabetes. Oxford Medicine Online. academic.oup.com, published November 2021
- Bariatric surgery sequelae. BMJ Best Practice. bestpractice.bmj.com, last reviewed May 2023
- Peterli R, Wolnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: The SM-BOSS
- Randomized Clinical Trial. JAMA 2018; 319(3):255–65. doi: 10.1001/jama.2017.20897
- Gronroos S, Helmio M, Juuti A, et al. Effect of laparoscopic sleeve gastrectomy vs Roux-en-Y gastric bypass on weight loss and quality of life at 7 years in patients with morbid obesity: The SLEEVEPASS Randomized Clinical Trial. JAMA Surg 2021; 156(2):137–46. doi: 10.1001/jamasurg.2020.5666
- Roux-en-Y Gastric Bypass and Sleeve Gastrectomy. University Hospitals Plymouth NHS Trust. plymouthhospitals.nhs.uk, published May 2023
- Laparoscopic gastric bypass. Medscape. emedicine.medscape.com, last updated April 2023
- Life after weight-loss surgery. Medline Plus. medlineplus.gov, last reviewed July 2021
- Obesity: identification, assessment and management. National Institute for Health and Care Excellence. nice.org.uk, last updated September 2022
- Eisenberg D, Shikora SA, Aarts E, et al. 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Indications for Metabolic and Bariatric Surgery. Obesity Surgery 2023; 33(1):3, published November 2022
- Bariatric Surgery. MSD Manuals. msdmanuals.com, last reviewed August 2021
- Anaesthesia explained. Royal College of Anaesthetists. rcoa.ac.uk, published March 2021
- O'Kane M, Parretti H, Pinkney J, et al. British obesity and metabolic surgery society guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery—2020 update. Obes Rev 2020; 21(11). doi: org/10.1111/obr.13087
- Romeijn M, Kolen AM, Holthuijsen DDB, et al. Effectiveness of a low-calorie diet for liver volume reduction prior to bariatric surgery: a systematic review. Obes Surg 2021; 31(1):350–56
- Laparoscopic gastric bypass periprocedural care. Medscape. emedicine.medscape.com, last updated April 2023
- Anaesthesia Explained: On the day of your operation. Royal College of Anaesthetists. rcoa.ac.uk, published March 2021
- Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. National Institute for Health and Care Excellence. nice.org.uk, last updated August 2019
- Decision making and consent. General Medical Council. gmc-uk.org, published November 2020
- Personal communication, Mr Peter Lamb, Consultant General and Upper Gastrointestinal Surgeon, July 2023
- Bariatric Surgery. Patient. patient.info, last updated April 2023
- Types of weight-loss surgery. National Institute of Diabetes and Digestive and Kidney Diseases. niddk.nih.gov, last updated September 2020
- Oxford Handbook of Operative Surgery (3rd ed). Oxford Medicine Online. academic.oup.com, published May 2017
- Thorell A, MacCormick AD, Awad S, et al. Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J of Surg 2016; 40:2065–83
- Roux en Y gastric bypass (RYGB). Royal Berkshire NHS Foundation Trust. royalberkshire.nhs.uk, published August 2020
- Oxford Handbook of Adult Nursing (2nd ed). Oxford Medicine Online. academic.oup.com, published June 2018
- Life After Bariatric Surgery. American Society for Metabolic and Bariatric Surgery. asmbs.org, last updated February 2021
- Aguas-Ayesa M, Yarnoz-Esquiroz P, Olazaran L, et al. Precision nutrition in the context of bariatric surgery. Rev Endocr Metab Disord 2023; Mar 17:1–13. doi: 10.1007/s11154-023-09794-5
- Alyahya RA, Alnujaidi MA. Prevalence and outcomes of depression after bariatric surgery: A systematic review and meta-analysis. Cureus 2022;14(6): e25651. doi. 10.7759/cureus.25651
- Going home after a laparoscopy (adult). Milton Keynes University Hospital NHS Foundation Trust. mkuh.nhs.uk, accessed June 2023
- Dumping syndrome clinical presentation. Medscape. emedicine.medscape.com, last updated June 2019
- Dumping syndrome. Medscape. emedicine.medscape.com, last updated June 2019
- Eating, Diet, & Nutrition for Dumping Syndrome. National Institute of Diabetes and Digestive and Kidney Diseases. niddk.nih.gov, last reviewed January 2019
- Common postoperative complications. Patient. patient.info, last updated November 2020
- Tips on a speedier recovery after surgery. University Hospital Southampton NHS Foundation Trust. uhs.nhs.uk, last reviewed March 2020
- Bariatric surgery. Medscape. emedicine.medscape.com, last updated March 2023
- Weight-loss Surgery Benefits. National Institute of Diabetes and Digestive and Kidney Diseases. niddk.nih.gov, last updated September 2020
- Bariatric surgery treatment and management. Medscape. emedicine.medscape.com, last updated March 2023
- Swallowable gastric balloon capsule for weight loss. National Institute for Health and Care Excellence. nice.org.uk, last updated November 2020



