Crohn’s disease
- Dr Derek Chan, Consultant Physician and Gastroenterologist
- Victoria Goldman, Freelance Health Editor
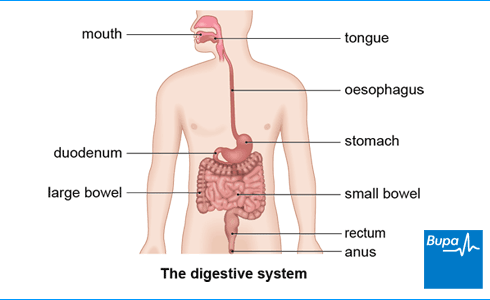
Crohn’s disease is a lifelong inflammatory bowel disease(IBD). It can affect any part of your digestive system, and causes tummy pain, persistent diarrhoea, and ulcers. Crohn’s disease is one of the two major types of IBD; the other is ulcerative colitis.
About Crohn's disease
Crohn’s disease can affect any part of your digestive system from your mouth to your anus (back passage). It most often causes inflammation in:
- the final part of your small bowel (ileum)
- the large bowel (colon)
The inflamed areas are usually separated by healthy areas of bowel called skip lesions. Crohn's disease affects about one in every 650 people in the UK.
Causes of Crohn's disease
Doctors don’t know exactly why some people get Crohn’s disease and others don’t. But it’s thought that several things can trigger the condition in susceptible people.
You’re more susceptible to Crohn’s disease if the condition runs in your family. If you’ve inherited the genes for Crohn’s disease, you may be more likely to get the condition if you encounter certain triggers. These triggers include:
- smoking
- an abnormal immune system reaction to certain bacteria and viruses in your bowel – this causes inflammation
- a recent gastroenteritis infection
- certain types and numbers of bacteria that live naturally in your digestive system
- eating lots of processed foods
Symptoms of Crohn's disease
If you have Crohn's disease, your symptoms are likely to come and go. The symptoms may be mild and occasional or they may be severe enough to affect your daily life. Some people with Crohn’s disease don’t have specific digestive symptoms, so they’re not diagnosed for many years.
The main symptoms and signs of Crohn's disease include:
- diarrhoea that doesn’t get better – sometimes it contains blood or mucus
- tummy pain, which can be severe
- feeling extremely tired
- losing weight for no reason
- a fever
- feeling generally unwell
- feeling or being sick (nausea and vomiting)
Crohn’s disease can also affect other parts of your body. You may have:
- mouth ulcers
- red and sore eyes
- a rash on your skin
- pain and swelling in your joints
If you have any of these symptoms, see your GP.
Diagnosis of Crohn's disease
Your GP will ask about your symptoms and examine you. They’ll also ask about your medical and family history. They may ask for a sample of your poo to check for:
- a bacterial infection
- faecal calprotectin – high levels of this substance in your poo suggest you may have inflammation in your bowel
Your GP may also take a blood sample to check:
- your iron levels to see if you have anaemia
- for other signs of inflammation
- If you’re very unwell with diarrhoea, bloody poo, a fever, fast heart rate or low blood pressure, your GP will refer you to hospital immediately. Otherwise, they may refer you to a specialist inflammatory bowel disease (IBD) team for more tests. These tests can include the following. A colonoscopy to look inside your bowel and take tissue samples.
- A CT scan or MRI scan to create images of the inside of your tummy. You may need to drink a liquid called contrast medium so your small bowel shows up more clearly.
- A capsule endoscopy. You swallow a small capsule containing a tiny video camera. The camera takes digital pictures inside your small bowel. Your doctor can see these pictures on a screen.
Self-help for Crohn's disease
There are some things you can do to help ease your symptoms.
If you smoke, speak to your pharmacist or GP about the best ways to stop smoking. Smoking makes you more likely to:
- have regular flare-ups
- need surgery to treat Crohn’s disease
Diet and Crohn’s disease
If you have Crohn’s disease, it's important to eat a healthy, balanced diet to make sure you get all the nutrients you need. There’s no specific diet for Crohn’s’ disease. But you may find that certain foods – such as those high in fibre – can make your symptoms worse.
You may find it helpful to keep a food diary to see if anything in particular triggers your symptoms. Click to open a PDF version of Bupa's food and symptoms diary (PDF, 1.4MB) . Speak to a dietitian before you stop eating any foods because you may miss out on essential nutrients.
Your doctor may recommend a liquid diet (enteral diet) during a flare-up to ease your symptoms. Liquid diets are easier to digest than normal food and will give you all of the essential nutrients you need. They may also help to reduce inflammation in your digestive system.
Treatment of Crohn's disease
There’s no cure for Crohn's disease, but different treatments can help to ease your symptoms. It’s important to keep Crohn's disease under control to prevent complications and stop your symptoms from getting worse.
The right treatment for you will depend on your symptoms and how severe they are.
- If you have mild Crohn’s disease, you may need to take medicines only when your symptoms flare up. Or you may not need any medicines.
- If your Crohn’s disease is worse, you may need to take medicines every day to prevent another flare-up.
- If you have very severe symptoms, you may need to go into hospital for treatment.
A specialist inflammatory bowel disease (IBD) team will support you. Your team will include a specialist nurse and doctor. It might also include a surgeon, a pharmacist, a dietitian and a psychologist to cover all aspects of your care.
Medicines for Crohn’s disease
You may need to take just one medicine or several medicines. It’s important to keep taking your medicines to keep your symptoms under control.
Your doctor may prescribe a corticosteroid (for example, prednisolone or budesonide). These ease inflammation. You usually only take them for a short time during a flare-up. This is because corticosteroids can cause side-effects such as acne, depression, high blood pressure, and diabetes.
If you have two or more flare-ups in 12 months, your doctor may prescribe an immunosuppressant (for example, azathioprine, mercaptopurine, or methotrexate). These medicines dampen down your immune system to reduce inflammation, but this can make you more likely to catch infections.
If the area around your anus is affected by Crohn’s disease, your doctor may offer you antibiotics such as metronidazole or ciprofloxacin. These may help to prevent or treat an infection.
If other treatments don’t help, your doctor may prescribe biological therapies such as:
- infliximab
- adalimumab
- vedolizumab
- ustekinumab
- upadacitinib
Your doctor can give you more information about these medicines.
Other medicines
Your doctor may suggest you take medicines to ease specific symptoms such as diarrhoea, constipation or cramping pains. You may also need to use medicines for other symptoms such as mouth ulcers.
If you need pain relief, you can take over-the-counter painkillers such as paracetamol. But don’t take non-steroidal anti-inflammatory medicines (NSAIDs) such as ibuprofen or aspirin, because these can make your symptoms worse.
Always read the patient information leaflet that comes with your medicine. If you have any questions, ask your pharmacist or doctor for advice.
Surgery for Crohn’s disease
Surgery can’t cure Crohn’s disease. But your doctor may suggest you have an operation if:
- you’ve recently been diagnosed, and Crohn’s disease is only in the end of your small bowel (before it turns into the start of your large bowel)
- you’ve tried several different medicines, and these haven’t worked
- you have severe inflammation – you may have an operation to remove a part of your bowel that’s very inflamed
- your surgeon needs to widen areas where your bowel has narrowed
- you have complications of Crohn’s disease such as an abscess or fistula
Complications of Crohn's disease
- Crohn’s disease may make you more likely to have other problems with your digestive system, including the following.
- A fissure . This is a cut in the wall of your anus. It can hurt and bleed when you go to the loo.
- A stricture (narrowing) in your bowel. This can block your bowel. It can cause pain, vomiting, and swelling in your tummy.
- An abscess (collection of pus). Severe inflammation in your bowel wall can form an ulcer. If the ulcer creates a hole, this can get infected and lead to an abscess.
- A fistula. This is a small tunnel between a hole in your bowel and surrounding tissues. It may connect your bowel to other parts of your body, such as your bladder, vagina, or skin.
- Malnutrition and anaemia. Damage to your bowel can affect how well your body absorbs vitamins and minerals (such as iron, folic acid, and vitamin B12) from food.
- Bowel cancer. It’s important to have your bowel checked regularly because you’re more likely to get bowel cancer in the future.
Crohn’s disease can make you more likely to get osteoporosis . Osteoporosis makes your bones become fragile and weak. You may need to have some tests to check your bone density and assess your risk of a bone fracture. Some corticosteroid medicines can also increase your risk of osteoporosis. If you take corticosteroids regularly, you may need to take calcium and vitamin D supplements to keep your bones healthy.
Crohn’s disease can also delay puberty in children who have the condition.
Living with Crohn's disease
Crohn’s disease affects everyone differently. If your symptoms are mild or clear up for a while, this may have little effect on your day-to-day life. But when you have a flare-up, you may need to take time off work or cancel social arrangements. If you tell your friends, family, and work colleagues about your Crohn’s disease, they’ll be better able to support you.
If you have diarrhoea regularly, it can make your skin sore. So it’s important to look after your skin properly. Ask your doctor, specialist nurse or pharmacist for advice on how to do this.
If you find that certain foods make your Crohn’s disease worse, it can be hard to know what to eat. It may help if you eat small meals more frequently rather than a few large meals each day. Your doctor can refer you to a dietitian if you need support.
If Crohn’s disease stops you eating properly, you may lose weight and feel very unwell. Your doctor or dietitian may recommend you take dietary supplements to make sure you get all the essential nutrients your body needs.
Crohn’s disease can be hard to deal with, especially because it’s so unpredictable. Stress can make your symptoms worse so try to relax as much as you can. Relaxation therapies, meditation, yoga, or whatever helps you to relax (for example, listening to music) may help to reduce the risk of a flare-up.
Rest if you’re feeling tired or having a flare-up. But try to do some form of activity every day if you can because it’s good for your health.
If you have a long-term medical condition such as Crohn’s disease, it can make you feel down. It can affect your relationships, and may lead to depression or anxiety. It’s important to discuss your feelings with your doctor or specialist nurse. You may find it helpful to see a counsellor or join a support group to meet other people who have Crohn’s disease.
Lots of things can trigger Crohn’s disease in susceptible people. Triggers include smoking, having certain types of bacteria in your bowel or having an infection such as gastroenteritis.
For more information, see our section on causes of Crohn’s disease.
Crohn’s disease affects everyone differently. The symptoms tend to come and go. Some people have only occasional symptoms, but others have severe symptoms that really affect their life.
For more information, see our section on symptoms of Crohn’s disease.
The main symptoms of Crohn’s disease include diarrhoea that doesn’t get better, tummy pain, feeling extremely tired, and losing weight for no known reason. You may also feel generally unwell.
For more information, see our section on symptoms of Crohn’s disease.
Doctors don’t yet know exactly why some people have Crohn’s disease. But you’re more likely to have the condition if it runs in your family. If you inherit the genes for Crohn’s disease, a specific trigger (for example, smoking) may cause it.
For more information, see our section on causes of Crohn’s disease.
Did our Crohn’s disease information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Crohn’s disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2020
- Bannaga AS, Selinger CP. Inflammatory bowel disease and anxiety: links, risks, and challenges faced. Clin Exp Gastroenterol 2015; 8:111–17. doi: 10.2147/CEG.S57982
- Overview of inflammatory bowel disease. MSD Manuals. msdmanuals.com, reviewed/revised November 2023
- Crohn’s disease. BMJ Best Practice. bestpractice.bmj.com, last reviewed November 2023
- Crohn disease. MSD Manuals. msdmanuals.com, reviewed/revised November 2023
- Capsule endoscopy technique. Medscape. emedicine.medscape.com, updated November 2023
- Food. Crohn’s & Colitis UK. crohnsandcolitis.org.uk, last reviewed February 2023
- Colorectal surgery. Oxford Handbook of Clinical Surgery. 5th ed. Oxford Academic. academic.oup.com, published November 2021
- Crohn’s disease: management. National Institute for Health and Care Excellence (NICE). NICE guideline NG219. published May 2019. www.nice.org.uk,
- Crohn disease. Medscape. emedicine.medscape.com, updated July 2019
- IBD standards. IBD UK. ibduk.org, accessed January 2024
- Crohn’s disease. NICE British National Formulary. bnf.nice.org.uk, last updated December 2023
- Prednisolone. NICE British National Formulary. bnf.nice.org.uk, last updated December 2023
- Azathioprine. NICE British National Formulary. bnf.nice.org.uk, last updated December 2023
- Inflammatory bowel disease. Colorectal Surgery. 2nd ed. Oxford Academic. academic.oup.com, published July 2021
- Crohn’s disease. Patient. patient.info, last updated August 2019
- Anal fissure. Medscape. emedicine.medscape.com, updated March 2023
- Osteoporosis – prevention of fragility fractures. Scenario: management. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2023
- Crohn’s disease. Crohn’s & Colitis UK. crohnsandcolitis.org.uk, last reviewed April 2021
- Diarrhoea. Crohn’s & Colitis UK. crohnsandcolitis.org.uk, last reviewed December 2023
- Mental health and wellbeing. Crohn’s & Colitis UK. crohnsandcolitis.org.uk, last reviewed February 2023
- Fatigue. Crohn’s & Colitis UK. crohnsandcolitis.org.uk, last reviewed April 2022
- Upadacitinib. NICE British National Formulary. bnf.nice.org.uk, last updated December 2023



